Mammography
What are the common clinical problems presenting as breast mass?
Common breast masses are:
What is the utility of the following imaging studies in the evaluation of breast mass?
- Mammography
- Ultrasound
- CT
- MR
- Thermography
Answer
- Mammography
- Is the imaging technique of choice for investigation of any palpable breast mass?
- Mammography is the gold standard imaging procedure for detection of early cancer.
- It is complementary to physical examination.
- Each method can detect tumors not detected by the other.
- Useful to guide diagnostic procedures.
- Ultrasound
- Is useful to distinguish a cyst from a solid mass and should not be relied for cancer screening.
- There is increasing use of ultrasound as a supplemental procedure following mammography to evaluate breast masses.
- Useful to guide diagnostic procedures.
- CT, Nuclear medicine scans and Thermography have no significant role in the evaluation of breast masses as of now.
- MR: New developments in evaluating the utility of this imaging modality is on going.
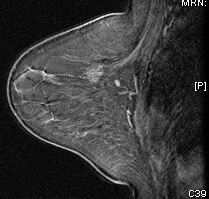 |
MR |
How is mammography done? What are the views?
Answer
- Cranio-caudal (top to bottom) view
- Medio-lateral oblique views: (MLO) for better visualization of tail of breast
- "Spot" views and magnification views can sometimes be used as well.
What is the primary utility of mammogram?
Answer
- The primary purpose of mammogram is to detect breast cancers.
- It is useful in the evaluation of palpable breast mass.
- It is a useful to guide diagnostic procedures.
How does mammogram differ with age?
Answer
- In young women, the breast may be dense.
- As women age there is fatty infiltration of the breast associated with atrophy of glandular tissue.
- Fat is lucent and is dark in mammogram.
- Glandular tissue and cancer are dense and white in mammogram.
- Hence, it is difficult to distinguish cancer from normal dense glandular tissue in young
women but fatty breast forms a good contrast for Cancer.
What are the primary and secondary mammographic signs of malignancy?
Answer
- Primary:
- Mass
- A spiculated mass is a common mammographic appearance.
- Calcifications
- Micro calcifications may be seen on mammography in at least 30% of cases of invasive carcinoma.
- They are 1 mm or less and sand-like.
- The calcifications may represent necrotic debris.
- Developing density
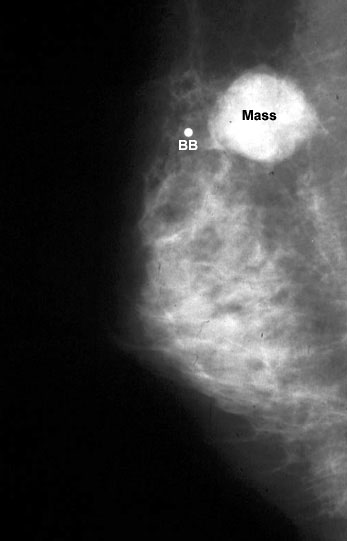 |
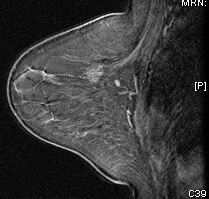
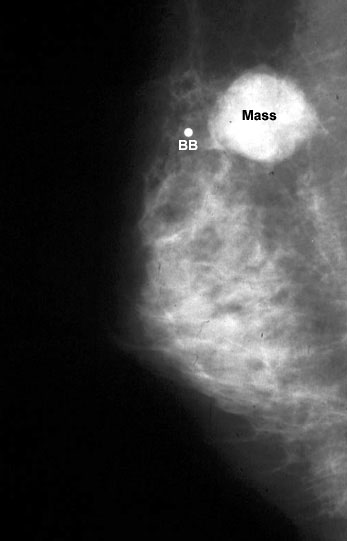
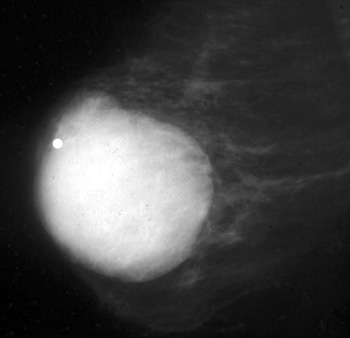
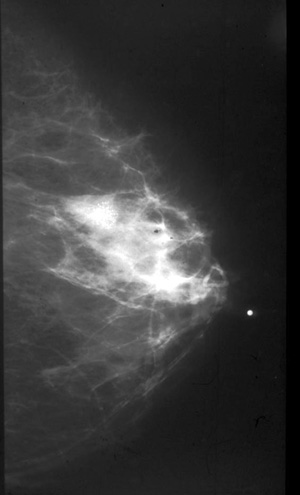
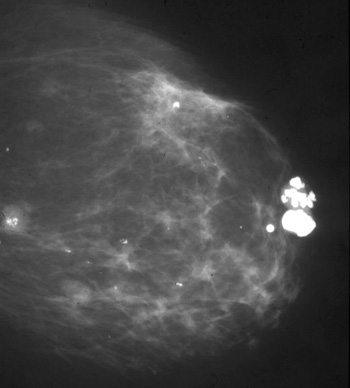
30 year old:
Smooth mass is infiltrating ductal carcinoma medullary type .
THe BB indicates that it is palpable. |
- Secondary:
- Architectural distortion
- Skin thickening or retraction
- Nipple and areolar thickening
- Abnormal ductal patterns
- Lymphadenopathy
- Asymmetry of the breast tissue
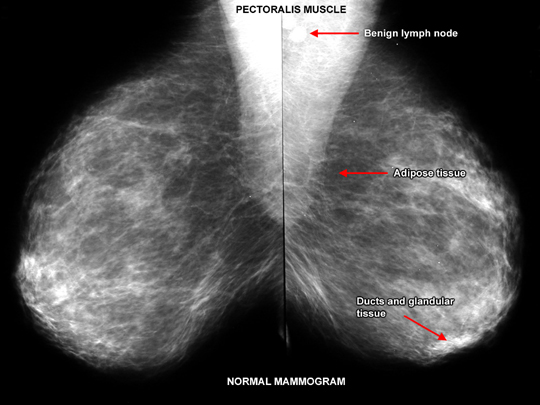
Normal mammogram
What is the most common type of breast cancer?
Answer
- 65-80% Invasive ductal carcinoma arises from the epithelium of the breast ducts.
- 03-14% Lobar carcinoma Invasive lobular carcinoma arises from the acini of breast lobules.
- 02-08% Tubular carcinoma
- Less than 1% of invasive breast cancers are sarcomatous or other mesenchymal origin.
What are the mammographic findings of invasive ductal carcinoma?
Answer
- Irregular mass
- New calcifications
- Calcifications are sand like
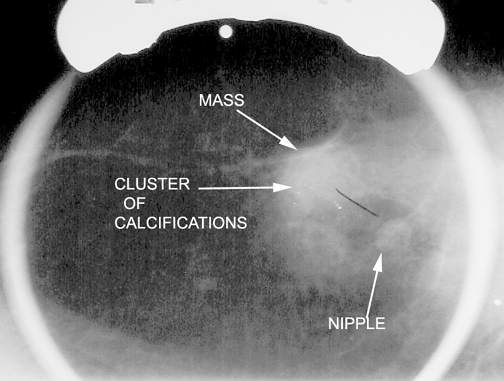
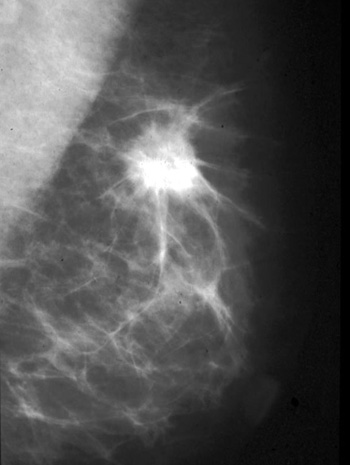 |
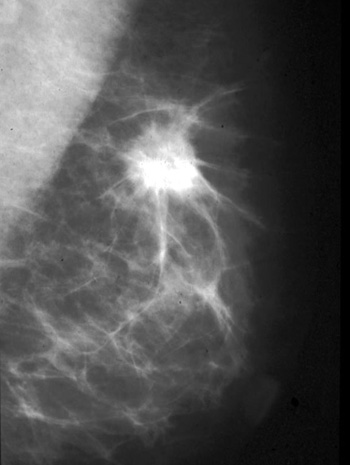
56 yr old :
Spiculated mass in upper breast indicating infiltrative ductal carcinoma. |
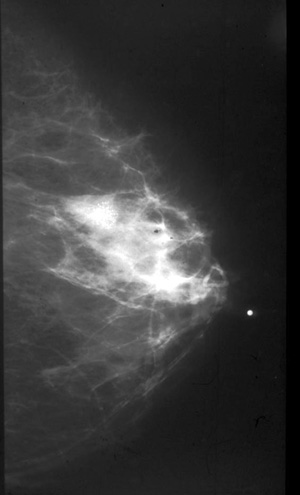
 |
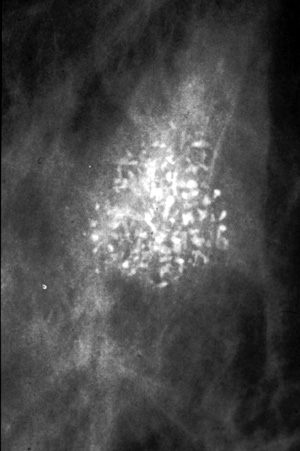 |
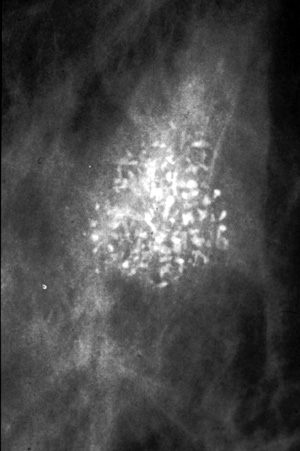
| Irregular clustered microcalcifications of ductal carcinoma in situ. |
Close up |
What are the mammographic findings of invasive lobar carcinoma?
Answer
What is the role of radiologist in biopsy of breast mass?
Answer:
- Core biopsy with stereotactic or ultrasound guidance.
- The lesion can be localized by the radiologist for biopsy and/or resection with mammographic or ultrasound guidance.
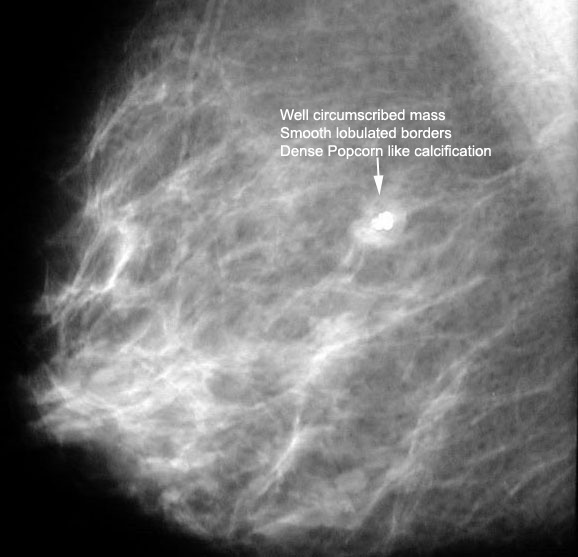
What is the classical appearance of fibroadenomas on mammography?
Answer:
- A fibroadenoma appears as a well-circumscribed round or oval mass with well-defined borders.
- They may be multiple and bilateral.
- It may have the appearance of a dense, popcorn-like calcification on mammogram.
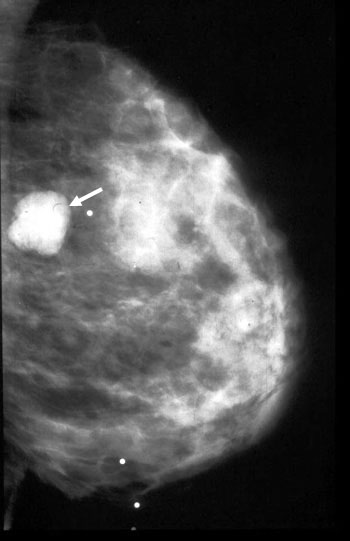
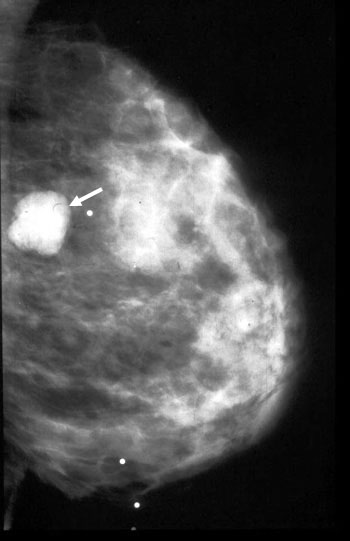 |
Fibroadenoma
35 year old:
Palpable smooth benign type mass. |
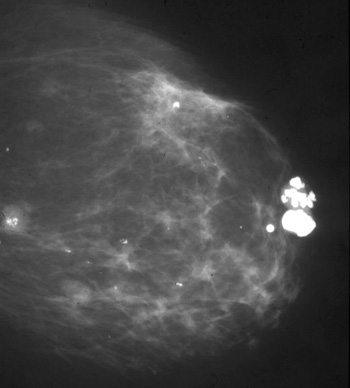
 |
Fibroadenoma
64 year old:
Palpable well delineated mass with irregular "pocorn" calcification. |
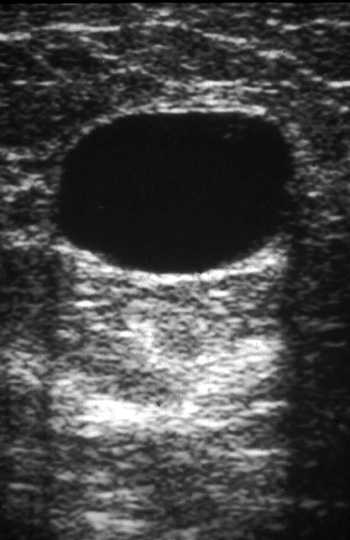
What is the classical appearance of cyst on mammography?
Answer
- Well defined mass
- Round
- No calcifications
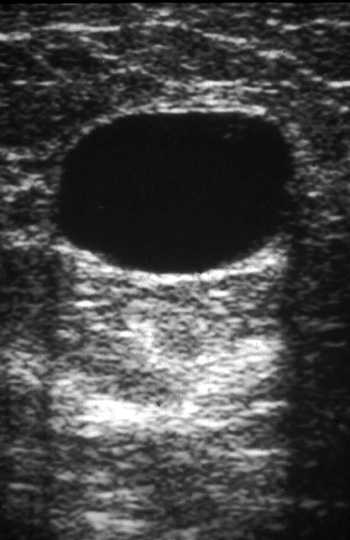 |
Ultrasound
Cyst Smooth anechoic mass with enhanced through transmission.
White echoes posterior to cyst. |
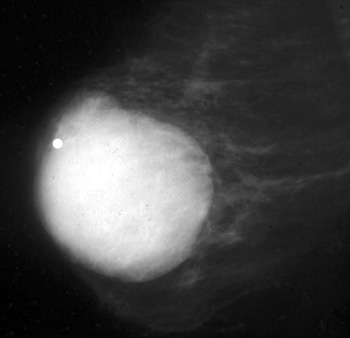 |
Mammogram
Cyst
Smooth benign type palpable mass. |
What is the most effective modality for the detection of breast cancer ?
- Clinical breast exam
- MRI
- Mammography
- Ultrasound
Answer
While all of the above modalities can potentially detect breast cancer, mammography is still the gold standard for early detection.
What are the risk factors for breast cancer?
The main risk factors for breast CA are:
- Family history of a first degree relative
- Previous history of contralateral breast cancer
- Early menarche
- Late menopause
- Nulliparity
- History of endometrial carcinoma
- Increasing age: The probability of developing breast cancer over 10 years starting
- at age 30 is about 0.4%.
- between 40-50 is about 1.5%.
- between 50-60 is about 2.8%.
- between 60-70 is about 3.6%.
Birth control pills and smoking are not risk factors (this is frequently asked on USMLE).
What conditions give rise to false positive suspicion for cancer breast?
Answer
Several benign breast conditions can produce a spiculated density which may be indistinguishable on mammography from carcinoma.
Spiculated mass density has been encountered in:
- Post-biopsy scarring
- Traumatic fat necrosis
- Breast abscess
- Sclerosing adenosis
- Radial scar
Screening mammogram reveals a suspicious lesion for cancer in left breast. No mass is palpable. How would you proceed?
Answer
- Core biopsy of stereotactic or ultrasound guidance; or
- Excision biopsy
- Radiologist performs needle localization procedure first.
- Breast is compressed with holder that has coordinates on the sides, and mammogram is obtained.
- A thin needle is placed in the lesion through coordinates.
- A blue dye is injected at the site.
- A thin hooked wire is passed to the lesion where it gets fixed.
- The needle is withdrawn leaving the wire in place.
- Surgeon removes the tissue around the wire tip.
- The biopsy specimen is x-rayed to make sure that the suspicious lesion was removed.
CASE 1
A 24 y/o woman comes to the office with a chief complaint of lumps in her breast. On exam, you find lumps that feel cystic in nature. The patient has no risk factors for breast cancer. What would be your advice to this young lady?
Answer:
- Ultrasound can be done.
- No intervention needed at this time. Most likely cause is fibrocystic change.
- Fibrocystic change is the single most common disorder of the breast. It occurs secondary to hormonal imbalances and primarily affects women between the ages of 20 and 40. Large cysts may appear as densities on mammogram, but fibrocystic changes can usually be diagnosed by disappearance of the mass after fine needle aspiration of the cyst contents.
CASE 2
CHIEF COMPLAINT: “I feel a lump in my breast”
HISTORY: A 36 year old female presents with a palpable mass in her left breast. She first noticed the mass one week ago while taking a shower. The mass is not painful, and the breast skin, nipples, and areola appear to be normal. There is no nipple discharge.
She is a healthy, active woman with an unremarkable medical history. She cannot recall any recent trauma to her chest, and denies a family history of breast cancer. The patient's obstetric/gynecologic history includes the following information: menarche age 12, menses occur regularly every 28 days and last for 5 days. She is gravida 0.
PHYSICAL EXAM: The breasts are examined with the patient in sitting and supine positions. The breasts are small and symmetrical. The contour of each breast is smooth; there is no evidence of dimpling, retraction, or edema. The nipples and areola are pink-tan and non-eczematous. Palpation reveals a well-circumscribed, firm mass in the lower-outer quadrant of the left breast. The mass is non-tender, movable, and its margins are easily distinguished. Estimated size of the mass is 1.5-2.0 cm in diameter. Compression of the nipples reveals no discharge. The remainder of the exam is without abnormality.
Q: Which one of the following imaging techniques is indicated to evaluate this palpable breast mass: ultrasound, mammogram, or MRI?
- Mammography is the imaging technique of choice to investigate a palpable breast mass in a woman age 30 and older.
- Ultrasound is the preferred test for women less than age 30 because the denser breast tissue on mammography makes it difficult to distinguish a lesion from the adjacent fibroglandular tissue.
Q: Fibroadenomas usually have what appearance on mammography?
- A fibroadenoma appears as a well-circumscribed mass.
- Its borders are smooth and round, oval, or nodular.
- They may be multiple and bilateral.
- It may have the appearance of a dense, popcorn-like calcification on mammogram.
CASE 3
CHIEF COMPLAINT: “I have a lump in my breast”
HISTORY: A 71 year old female presents with a mass in the upper, outer portion of her left breast. She first noticed the mass “several months ago” while bathing. She did not seek medical attention at the time because “I thought it would just go away if I left it alone.” She decided to come in today because the mass is becoming “harder, and getting larger.”
The patient states “the lump can sometimes be painful when I touch it.” She denies any nipple discharge or changes of the areola and nipples. The patient's obstetric/gynecologic history includes the following information: menarche age 11, menses occurred regularly until age 56; patient is now postmenopausal. Her last mammogram was >10 years ago.
PHYSICAL EXAM: The breasts are examined with the patient in sitting and supine positions. The breasts are large, pendulous, and asymmetric. The left breast is larger than the right breast, showing fullness in the upper, outer quadrant. The skin of the upper, outer quadrant is dimpled. Palpation of the left breast reveals a large, firm mass. The mass is non-tender, fixed to the anterior chest wall, and has margins that are not quite clear. Estimated size of the mass is 5.0 cm in diameter. The left axilla contains 2-3 enlarged, firm, non-tender lymph nodes. The nipples and areola are pink-tan and non-eczematous. Compression of the nipples reveals no discharge. Exam of the opposite breast and axilla reveals no abnormalities.
Q: What is the most common type of breast cancer?
- Invasive ductal carcinoma, which arises from the epithelium of the breast ducts, accounts for nearly 94% of invasive breast cancers.
- Invasive lobular carcinoma arises from the acini of breast lobules and accounts for 5.5% of cases.
- Less than 1% of invasive breast cancers are sarcomatous or other mesenchymal origin.
Q: What is the most common mammographic appearance of invasive carcinoma?
- A spiculated mass is the most common mammographic appearance.
- In addition, microcalcifications may be seen on mammography in at least 30% of cases of invasive carcinoma.
- The calcifications may represent necrotic debris.
Q: Several benign breast conditions can produce a spiculated density, which may be indistinguishable on mammography from carcinoma. List some of these benign conditions.
- Post-biopsy scarring
- Traumatic fat necrosis
- Breast abscess
- Ssclerosing adenosis
- Radial scar
can all potentially be seen as a spiculated density.
Case 4
A 29 y/o woman comes to the office for a routine physical examination. She is gravida 1, para 1.
Her social history is significant for both smoking (1ppd) and occasional EtOH. A significant amount of her dietary intake is from fast food restaurants. Her family history is significant for breast cancer (mother). The patient is also on orthotricyclin for birth control. Please identify this woman's risk factors for breast cancer.
Answer:
- This patient's risk factors include family history.
- NOTE: Birth control pills and smoking are not risk factors (this is frequently asked on USMLE)
REFERENCES
- Grainger & Allison's Diagnostic Radiology: A Textbook of Medical Imaging, 4 th Edition . 2001. Churchill Livingstone, Inc., pp. 2240-2273.
- Novelline, Robert A. Squire's Fundamentals of Radiology 5 th Edition . 1999. Harvard University Press, Cambridge, MA, pp. 406-410.
- U.S. Preventive Services Task Force (USPSTF) Recommendations and Rationale: Screening for Breast Cancer. 2002.