|
COLLAGENS |
|
TYPE I COLLAGEN: the most abundant collagen of mature scar tissue present in portal fields and fibrous septa. |
|
TYPE III COLLAGEN: Also abundant as type I and very abundant in distensible organs such as arteries and skin. |
|
TYPE IV COLLAGEN: this type is present in the matrix surrounding epithelial cells, therefore in the liver is in the sinusoids and in the basement membranes of vessels and bile ducts. |
|
TYPE V COLLAGEN: fine collagen fibrils which probably constitute the core of larger fibrils. It increases in cirrhosis where they surround hepatocytes. |
|
TYPE VI COLLAGEN: it is found throughout the connective tissue and its function is probably that anchoring structures to collagen fibers. |
|
TYPE VII COLLAGEN: the largest collagen apparently functions as an anchoring agent between basement membranes and underlying stroma. Collagens type II, VIII, IX, X, XI, XII, and XIII are not found in the liver. |
|
GLYCOPROTEINS |
|
LAMININ: is a glycoprotein that is distributed with collagen IV. It is increased in perisinusoidal fibrosis. It can be measured in the serum and correlates with the degree of fibrosis. Consists of 3 polypeptide chains. |
|
FIBRONECTIN: consists of 2 polypeptide chains. It mediates adhesion of collagen, fibrin and heparin to cells, therefore it is involved in the organization of thrombi and in wound healing inducing attachment of these structures to cells. |
|
ENTACTIN: is a polypeptide apparently a facilitator of laminin. |
|
UNDULIN: A 3 chain polypeptide associated with types I and II collagen, thus present in portal fields. It might facilitate the cross linkage of these fibers. |
|
ELASTIN: Present in the wall of blood vessels and in the capsule and increases in fibrosis. |
|
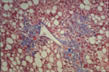
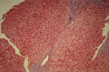
Central fibrosis, mild
|
Fig.66 - CENTRAL FIBROSIS, MILD: The mild form consists of deposition of fine collagen fibers in the sinusoids of the pericentral lobular region. This form is called "chicken wire fibrosis".
|
|
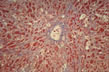
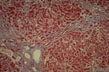
Central fibrosis, severe
|
Fig.67 - CENTRAL FIBROSIS, SEVERE: This form of fibrosis mostly occuring in alcoholics goes under the name of "sclerosing hyalin necrosis". It consists of wide pericentral areas of fibrosis that may extend to portal fields.
|
|
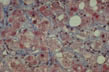
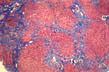
Portal and periportal fibrosis
|
Fig.68 - PORTAL AND PERIPORTAL FIBROSIS: Fibrous expansion of portal fields with fibrosis extending along the terminal centracinar portal veins assuming the appearance of "stellate" fibrosis. Expansion and branching of normal portal fields must not be confused with pathological portal fibrosis which contains inflammatory cells.
|
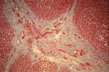
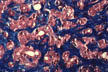
Bridging fibrosis
Central-central
|
Fig.69 - BRIDGING FIBROSIS: Central-central. Connects central veins with central veins. It is rare and occuring mostly in chronic passive congestion as in this case.
|
Bridging fibrosis
Porto-portal
|
Fig.70 - BRIDGING FIBROSIS: Porto-portal. This form is common and usually associated with porto-central fibrosis. It follows a portal inflammation that extends to the terminal, centroacinar, portal venules.
|
Bridging fibrosis
Porto-central
|
Fig.71 - BRIDGING FIBROSIS: Porto-central. It occurs after centrolobular necrosis and produces new vascular connections between portal fields and central veins which may lead to cirrhosis. It is the most severe form of bridging necrosis and fibrosis and is most of the times associated with porto-portal fibrosis.
|