Case Questions:
- What are commonly accepted indications for intubation?
- BiPAP or CPAP is commonly used in patients suffering from an acute exacerbation of COPD, prior to intubation.
- How does BiPAP help in this situation?
- What is the approximate number needed to treat to prevent one intubation?
- Besides its use in acute on chronic respiratory failure (i.e., COPD exacerbations), what are the clinical settings in which CPAP and/or BiPAP have been studied and shown to be potentially advantageous?
- After intubation, what ventilator settings would you recommend? Why?
Mode: _____________
TV: _____________
PEEP _____________
Rate: _____________
FIO2: _____________
- Describe the difference between pressure-cycled and volume-cycled ventilators.
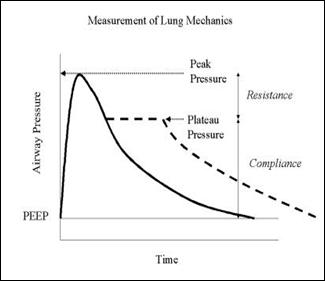
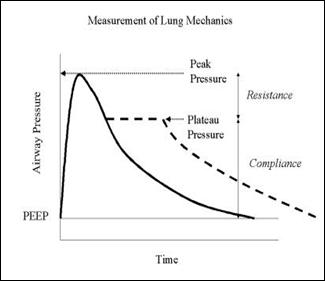
- How would you assess the appropriateness of your ventilator settings in addition to (and while waiting for) the results of an ABG?
- What would be your explanation if immediately after intubation the patient's BP were?
High ?
Low ?
- What type of respiratory failure is a patient with COPD most likely to develop and why?
- What is the underlying mechanism of hypoxemia in patients with COPD? Is the hypoxemia typically easily responsive to supplemental oxygen or relatively refractory?
The patient stabilizes on the following settings: a/c = 16, TV = 500 cc, FiO2 = 40 %, PEEP = 5 cm H2O, and I:E = 1 to 3. The observed respiratory rate is 28, peak pressure is 55 cm H 2 O and plateau pressure = 15 cm H 2 O. Pulse oximeter registers a saturation = 95 %. In addition, the patient's BP, which was 160/85 shortly after intubation is now 115/80, and the HR is 132.
- Based upon the available data, what is the static compliance?
- Is the peak to plateau pressure gradient most consistent with increased airways resistance or diminished lung compliance?
- What is the most likely explanation for the drop in blood pressure?
- What ventilator adjustments would be expected to reduce auto-PEEP (intrinsic Peep or dynamic hyperinflation) if present?
With appropriate intervention, the patient initially stabilizes. However, over the next several days, he deteriorates and, on your next call night, you again are called to assess the patient because of decreasing oxygen saturation. On your evaluation the patient is restless, BP = 165/80, HR = 116, RR = 26, and T = 385. Otherwise the physical exam is notable only for occasional basilar crackles. The patient's ventilator is set on a/c = 12, TV = 500 cc, FiO2 = 60 %, and PEEP = 5 cm H2O. You determine the peak and plateau pressures are 55 and 30 cm H2O respectively. There is no significant auto-PEEP. CXR from earlier in the day reveals diffuse infiltrates which are new from admission. ABG reveals a pH = 7.34, PCO2 = 44, and pO2 = 52. CBC reveals a hgb = 9.0.
- What is the patient's calculated static compliance?
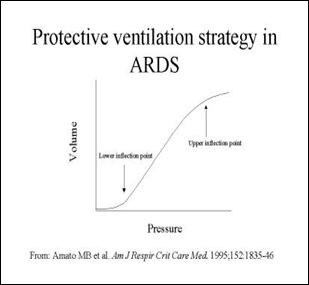
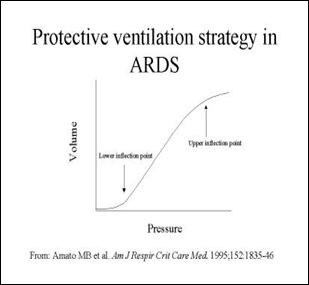
- What are the clinical criteria for ARDS?
- What general type of respiratory failure do patients with ARDS suffer from?
- What is the underlying mechanism of hypoxemia in patients with ARDS? Is the hypoxemia typically easily responsive to supplemental oxygen or relatively refractory?
- What might you do to increase the PaO2 in this patient?
The patient in this case originally presented with Acute Hypoventilatory Respiratory Failure that was then complicated by Acute Hypoxemic Respiratory Failure secondary to low-pressure pulmonary edema (i.e., ARDS) .
- How would your management differ in the case of Acute Hypoxemic Respiratory Failure secondary to high-pressure pulmonary edema (i.e., secondary to CHF) ?
The management of a patient in Acute Hypoventilatory Respiratory Failure secondary to Status Asthmaticus is extremely challenging. Pharmacologic strategy emphasizes bronchodilator therapy and corticosteroids, with the occasional use of magnesium sulfate infusions and/or theophylline.
- Describe the typical ventilator strategy employed when managing a patient in status asthmaticus, focusing on the TV and flow rate as well as targeted pH/PaCO2.
- Describe some of the complications associated with mechanical ventilation.
- What would be your immediate response if faced with sudden desaturation/difficulty breathing of a mechanically ventilated patient .
- List the standard "weaning parameters" and the values for each which predict successful weaning.