1. If the patient developed a complication
requiring hospital admission, what type of isolation would be required?
Patients with VZV infection, especially
chickenpox, are very contagious. Persons without a history of chickenpox are
susceptible. Chickenpox in adults can be more severe, with an increased
incidence of complications. Hospitalized patients with chickenpox must be in
negative airflow respiratory isolation, and strict infection control
measures regarding skin contact (hand-washing, use of gloves and gowns,
etc.) must be implemented.
Hospital workers without a history of
chickenpox or those already known to be seronegative for VZV should not come
into contact with these patients.
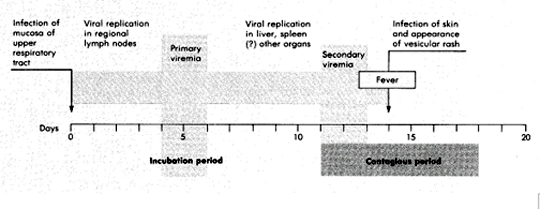
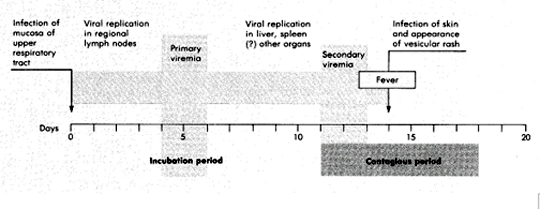
2. What is known about the pathogenesis of the infection?
3. The pediatrician made a clinical
diagnosis. Should laboratory tests be run to confirm the diagnosis?
No. The diagnosis of chickenpox is often
made on the basis of clinical findings alone. For laboratory confirmation,
the virus can be isolated but this is rarely requested because the virus
grows slowly in tissue culture, often requiring 2 to 3 weeks for isolation.
Rapid and sensitive immunofluorescence assays are available and can be
performed on scrapings taken from vesicular lesions. A Tzanck test can be
performed, but is insensitive. The Tzanck test detects multinuclear giant
cells, a cell type characteristically seen with VZV and HSV infections.
4. Are there any effective anti-viral
agents that act against this virus?
Acyclovir is beneficial in treating
varicella in immunocompromised children with varicella, and may be useful in
adults and selected immunocompetent children with varicella.
Acyclovir (ACV) is a nucleoside analogue
of guanosine. ACV has selective action against those herpesviruses that
encode a Thymidine Kinase (TK). The viral Thymidine Kinase activates the
drug by phosphorylation, and host cell enzymes complete the process to the
triphosphate form. No initial phosphorylation occurs in uninfected cells,
and thus there is no active drug to inhibit cellular DNA synthesis or to
cause toxicity.

Activation of acyclovir (acycloguanosine)
in herpes simplex viral infected cells. Acyclovir is converted to
acycloguanosine monophosphate (acyclovir GMP) by the herpes-specific viral
thymidine kinase and then to acyclovir GTP by cellular kinases.
In herpesvirus infected cells, ACV
triphosphate competes with guanosine triphosphate and causes termination of the
growing viral DNA chain because there is no 3'-hydroxyl group on the ACV
molecule to allow chain elongation. The selectivity and minimal toxicity of ACV
is also due to its 100-fold greater utilization by the viral DNA polymerase than
by cellular DNA polymerase.
Mutations in either the herpesvirus TK or
polymerase can generate ACV resistant strains. These resistant strains are less
virulent but can still cause disease in immunocompromised patients.
Activity of ACV against herpesviruses directly
correlates with the capacity of the virus to produce TK. The order of TK
induction and ACV sensitivity is:
HSV-1 and HSV-2 > VZV>>EBV>>>CMV
5. Are there any long term consequences
associated with this viral infection? What bacterial superinfections may
occur with varicella? What are other complications of varicella?
Zoster (shingles) can occur later in life
as a result of reactivation of VZV from latent infection in ganglia.
Typically, skin lesions appear in a dermatomal distribution innervated by
the specific dorsal root or extramedullary cranial ganglia where VZV had
been latent. Pain often occurs with the rash and can persist even after the
skin lesions heal. This complication is more common in elderly patients.
Rarely, skin lesions disseminate beyond the primary dermatome involved. In
immunosuppressed patients, however, complicating viremia can occur with
dissemination to extradermatomal skin sites, lungs, liver, and central
nervous system. This latter condition is called disseminated zoster. Group A
streptococcus and staphylococcus aureus may cause superinfections following
varicella, including osteomyelitis, myositis, bacteremias, pneumonia and
toxic shock syndrome.
6. A new vaccine against VZV is available.
Describe it. Should the 3 year-old boy receive the vaccine or any other
therapy? What are the current recommendations for the use of the vaccine?
The VZV vaccine was licenced in March,
1995. If the boy was not vaccinated prior to his chemotherapy and has not
previously had varicella, he should receive VZIG (varicella immune globulin)
to help neutralize the virus infection.
Vaccine is generally not given to
immunosuppressed patients; however, it may be available through a research
protocol to children with ALL who have been in remission for 1 year.
7. Two weeks later, the patient=s mother
who did not have a history of chickenpox and is 39 weeks pregnant, develops
varicella. She develops respiratory distress and is admitted. The next day
she delivers the infant. What should be done for the baby and mother?
The mother should receive acyclovir. The
baby should receive VZIG (varicella immune globulin) to try to neutralize
the viral infection. If the treatment is successful, the baby may be
susceptible to VZV in later life. VZIG is recommended to infants whose
mothers have onset of chickenpox 5 days before and 2 days after delivery
(baby will have been viremic without adequate time for mother to give baby
VZV antibody).If the infant develops varicella despite VZIG, acyclovir
should be used to treat the baby because of the high morbidity and mortality
of these infections.
8. Two weeks after that, a nurse who cared
for the mother develops chickenpox. She thought that she had the illness,
but questioned her mother who reported that she had not. The nurse had been
at work for the past 2 days and had been on the Pediatric ward, caring for
children with hematologic malignancies. What action should be taken? What
could have been done to prevent this problem?
All exposed susceptible immunocompromised
children should receive VZIG. This problem could have been prevented if a
history of prior varicella were taken on all employees and a VZV IgG titer
performed on those without a history of varicella to check for immunity. All
non-immune personnel should be vaccinated with the live-attenuated vaccine.