Pancreatic Cancer
Q&A
1. What are the typical symptoms of pancreatic cancer?
- Often asymptomatic in early stages:
- Later symptoms may include:
- Weight loss
- Anorexia
- Epigastric discomfort
- Back pain
- Jaundice (only in cancer of the head of pancreas)
2. What percentage of patients present with pancreatitis as the first symptom of
pancreatic cancer?
3. What are the typical features of pain from pancreatic cancer and what does the pain
signify?
- pain exacerbated by recumbancy relieved when sitting up and leaning foreword
- signifies perineural invasion of the tumor- a poor prognostic indicator
4. What would polyuria and polydipsia in this patient signify?
5. Approximately what percentage of patients present with Diabetes as a sequelae of
pancreatic cancer?
6. At what age does pancreatic cancer present and is there a female/male predominance?
- Pancreatic cancer presents in the fourth to sixth decade
- Predominance in males
7.What are the risk factors for pancreatic cancer?
- Smoking
- High fat, low fiber diet
- Chronic calcified pancreatitis
- Occupational exposure to petroleum products, benzidine
8. Where is jaundice first seen?
At what serum bilirubin does it first become evident?
9. What is Virchow’s node?
- Left supraclavicular node
10. What is a Courvoisier gallbladder?
- Dilated gallbladder
- Associated with malignant biliary duct obstruction
11. What percentage of patients have a Courvoisier gallbladder?
- 50% of patients with carcinoma of the head of the pancreas
12. Why should the umbilicus and cul-de-sac be examined carefully?
- Metastatic peritoneal implants can be detected:
- Sister Mary Joseph nodes (umbilicus)
- Blumer’s shelf (cul-de-sac- palpable on rectal exam)
13. What serum diagnostic tests should be performed?
- CBC
- Electrolytes
- Liver function studies
- PT/PTT
14. What radiographic studies can be performed? Are any of these specific for
pancreatic cancer?
- Studies that image the pancreas
- Ultrasound
- Endoscopic ultrasound
- CT
- MRI
- Studies that image the biliary tree and pancreatic ducts
- Studies of vascular structures of the pancreas
- Celiac and mesenteric angiography
None of these tests are highly specific for pancreatic cancer. CT and ultrasound are
the least invasive and very sensitive for lesions >2 cm. However a smaller lesion may
not be seen. In this case endscopic ultrasound is a useful procedure.
15. What are the types of non-islet cell pancreatic cancer?
- Adenocarcinoma
- Lymphoma
- Cystadenocarcinoma
- Squamous cell carcinoma
- Acinar cell carcinoma
16. What is the most common type of pancreatic cancer?
- 90% of malignant exocrine tumors are duct cell adenocarcinomas
17. What is the prevalence of pancreatic cancer?
- 5th leading cause of cancer death
- 28,000 new cases diagnosed un the US each year
18. Why is vitamin K given?
- Bile is required for absorption
- Pts with biliary obstruction require vitamin K to maintain hemostasis
Review Question
What are the vitamin K-dependent clotting factors?
- II
- VII
- IX
- X
- Protein C
- Protein S
19. What percentage of patients have an anomalous origin of the right hepatic artery
and from what vessel?
- 15-20% have a right hepatic originating from the SMA
Review Question
From what artery does the right hepatic artery originate in the majority of the
population?
- Common hepatic (from the Celiac trunk)
20. Why is knowing the anatomical variation of the hepatic artery
important?
- When originating from the SMA it courses posterior to the head of the pancreas
- In this position it is at risk in a pancreatic resection
21. What is the staging of pancreatic cancer?
22. What is the pattern of spread of pancreatic cancer?
Two major patterns of spread occur:
- into regional lymph nodes
- local invasion of contiguous structures
23. Which pancreatic cancers can be resected for "cure"?
- small tumors (<2 cm)
- no local invasion
24. What are the findings at staging that predict unresectability?
- Tumors involving the body or tail
- Invasion of contiguous structures
- Invasion of the bile duct
- Involvement of celiac, hepatic, or superior mesenteric arteries
- Involvement of portal, splenic, or superior mesenteric veins
- Hepatic mets
- Peritoneal seeding
- Gross nodal mets
25. What are the techniques for pancreatic biopsy?
- Open Wedge biopsy
- Core needle biopsy
- Fine needle (CT guided)
26. What are the risks of biopsy?
- Open wedge biopsy have risk of pancreatitis and pancreatic fistula
- Core biopsy also has risk of developing fistula
- Fine needle has lowest complication rate (1-2%)
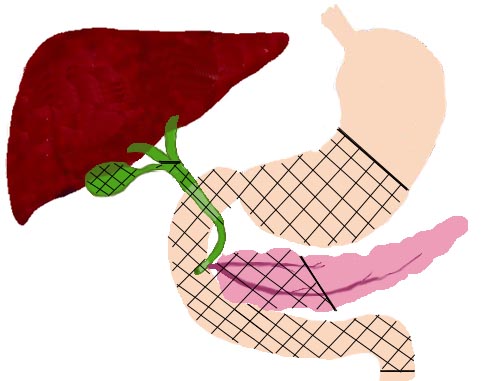
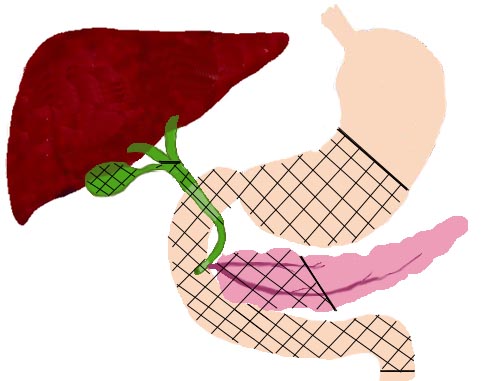
27. What is the most common resection performed for pancreatic cancer?
- Whipple procedure (pancreatoduodenectomy)
- Removal of:
- Gallbladder
- Common bile duct
- Duodenum
- Head of pancreas
- Pylorus
- Distal stomach
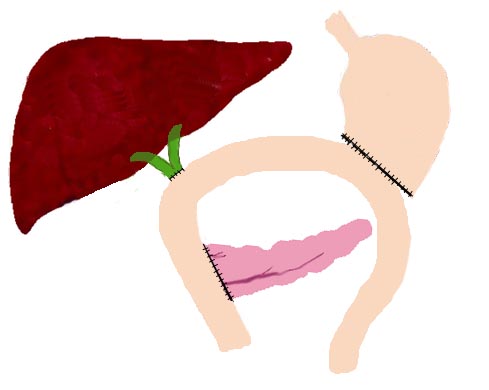
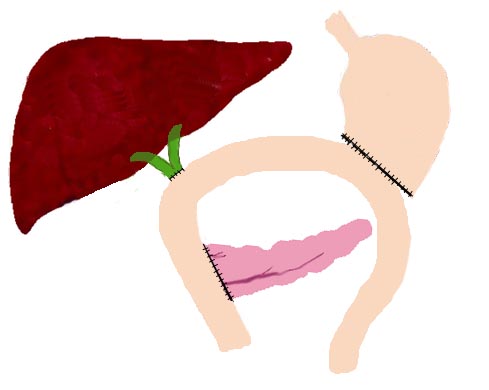
- Restoration of GI continuity via:
- Pancreaticojejunostomy
- Hepaticojejunostomy
- gastrojejunostomy
28. What is the rationale for total pancreatectomy?
- Total pancreatectomy was proposed in the 1960’s when overall survival rates from
pancreaticoduodectnectomy was low
- low survival rates presumed to be due to multicentricity of tumor
- now with improved technique mortality from both operations are equivalent
- disadvantages now outweigh advantages
- total pancretectomy allows dissection of more lymph nodes
- elimination of pancreaticojejunal anastamosis and its risk of leak
- disadvantages:
- requires removal of the spleen
- exocrine and endocrine dysfunction requiring insulin as well as digestive enzyme
supplementation
29. Is there a role for preoperative biliary tract decompression?
- Randomized prospective studies have shown that routine percutaneous transhepatic biliary
drainage does not reduce operative mortality and morbidity and may increase hospital stay.
- Biliary drainage is indicated in patients with biliary sepsis secondary to cholangitis
or in patients with major nutritional deficiencies because of severe biliary obstruction.
30. What palliative procedures for pancreatic cancer are currently available and what
are the advantages and risks of each?
1. Minimally invasive
- percutaneous transhepatic drainage catheter (PTC)
- advantage: constant access to the biliary system
- disadvantage: requires an external catheter.
- endoprothesis
- advantage: endoprotheses drain internally
- disadvantage: subject to obstruction by biliary sludge and require endoscopic surgery
for placement and revision.
2. Palliative surgery
- Biliary-enteric bypass with gastrojejunostomy
- Advantage: gastrojejunostomy prevents development of duodenal obstruction
- Disadvantage: an invasive procedure with associated operative risks
31. How common is duodenal obstruction?
- Approximately 6-30% of patients with nonresectable cancer will develop duodenal
obstruction.
32. What palliative procedures for pain control are available?
- Oral, transdermal medications
- Celiac ganglion blocks with 95% alcohol
- Celiac block can be performed at the time of surgery
- provides pain relief for 4-6 months.
Intraoperative external beam radiation
- may provide up to 4 months of pain relief in selected patients
33. What are the current operative morbidity and mortality rates for
pancreatoduodenectomy? For total pancreatectomy?
- Perioperative mortality rate from pancreatoduodenectomy is less than 5%.
- Mortality from total pancreatectomy is approximately equivalent, however it caries added
morbidity due to exocrine and endocrine dysfunction after resection
34. What are the major complications of pancreatoduodenectomy and total pancreatectomy?
Complications of pancreatoduodenectomy:
- Anastamotic leak
- Abscess
- Fistula
- Pancreatitis
- infection
Complications of total pancreatectomy:
- Same complications as above +
- Bleeding
- Hypoglycemia
35. Is there a role for adjuvant chemotherapy and radiation?
- Combination external beam radiation therapy and 5-fu may improve survival following
resection
- chemotherapeutic and radiotherapies also used for palliation of unresectable or
recurrent disease
- no increase in survival has been found in patients with inresectable disease
36. What are the current survival statistics for pancreatic cancer?
- Overall 5 year survival rate for all patients with resected periampullary tumors is
approximately 15-25%.
- The site of tumor origin has a large impact on survival.
- tumors of the duodenum, distal bile duct and ampulla are associated with 40-60% five
year survival
- carcinomas of the head of the pancreas are associated with a 5-25% five year survival
37. How would you
differentiate between obstructive, hemolytic, and hepatocellular forms of jaundice?
Obstructive jaundice:
Hemolytic jaundice:
Hepatocellular:
38. Differential diagnosis includes:
- choledocholithiasis
- neoplasm of the head of the pancreas
- neoplasm of the ampulla of vater
neoplasm of the duodenum