 |
 |
 |
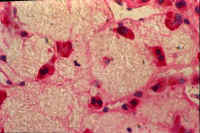 |
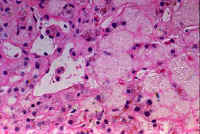
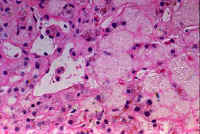
| Fig. 10-4. Normal hepatic veins | Fig. 10-4-2. Occluded hepatic veins | Fig. 10-4-3 .Congested sinusoids | Fig. 10-4-4.Lysed red cells in sinusoids |
Li-10-4
Disorders of hepatic veinsby Dr. E. ORFEI
CONTENTS
1-Occlusion of main hepatic veins (Budd-Chiari syndrome).
2-
Veno-Occlusive Disease of small intrahepatic veins (VOD).1- Occlusion of main hepatic veins (Budd-Chiariís syndrome
).In this condition the large hepatic veins emptying into the inferior vena cava are affected by a sudden thrombotic accident or a slow fibrous occlusion. At difference with Veno Occlusive Disease, here the occlusion occurs more frequently in the large hepatic veins at their entrance into the inferior vena cava. The causes are primary and secondary disorders of coagulation due to defects, diseases (ulcerative colitis), drugs (oral contraceptives) and neoplasms. The histology of the liver in early stages will reveal marked dilatation in the center of the central vein and pericentral sinusoids with perivenular fibrosis and signs of periportal regeneration with nodular changes. The dilated sinusoids will contain lysed erythrocytes at difference with passive congestion due to heart where the red cells are not lysed. In late stages there will be fibrosis and cirrhosis similar to liver in chronic cardiac failure.
If the occlusion is sudden and massive, the clinical signs are hyperacute, fulminant, with sudden massive ascites, abdominal pain and liver failure in a few days. If the occlusion is gradual these symptoms are attenuated and will develop within a month in acute cases and in a few months in chronic cases. Mortality is about 50% of cases within 3 years and very few cases thereafter.
EXAMPLES
Case no 1: 46 year old female was on oral contraceptives for 9 years. Suddenly she developed jaundice high serum transaminases and mild ascites. A needle liver biopsy was performed. She died 2 weeks later in liver failure in the time before the practice of liver transplantation. The findings of the liver biopsy are here illustrated.
 |
 |
 |
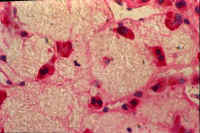 |
| Fig. 10-4. Normal hepatic veins | Fig. 10-4-2. Occluded hepatic veins | Fig. 10-4-3 .Congested sinusoids | Fig. 10-4-4.Lysed red cells in sinusoids |
Case no 2: 28 year old female began to use oral contraceptives after her second pregnancy. Two years later she developed gradual liver insufficiency with ascites, jaundice and signs of hepatitis. A liver biopsy revealed marked perivenular fibrosis. She died a year later with massive ascites. The liver was diffusely scarred. The large hepatic veins were totally obliterated. There was advanced cirrhosis.
2-Veno-occlusive disease (VOD)
This disease consists of occlusive fibrosis of small intrahepatc veins: centrilobular and sublobular venules. Lager veins and those affected by Budd-Chiari syndrome are spared.
Pathology:
There is concentric occlusion of the affected veins by loose connective tissue. The changes start with subendothelial edema and terminate with a scar replacing the vein. Severe congestion of the pericentral sinusoids accompanies this type of vascular occlusion. The lesion may resolve or produce centrolobular fibrosis, centro-portal bridging and cirrhosis. The changes are best demonstrated by connective tissue stains such as Mellory trichrome and silver impregnation. The lesion is not easily visible with H&E stain.
Pathogenesis.The initial change consists of blockage of blood flow in the pericentral sinusoids by fibrin and platelet aggregates. The blood can no longer reach the central vein, which develops intraluminal fibrosis by disuse. Fibrous occlusion by disuse is the mechanism operating in the occlusion of the ductus arteriosus in the heart of the neonate. ( Stirling at al. Archives Dis. Childhood. 37:535,1962).
Click on pictues to enlarge
Clinical presentation:
Acute form. Sudden ascites, liver enlargement and rapidly rising bilirubin heading to recovery or death.
Subacute form. Incomplete recovery of an acute form.
Chronic form. Fibrosis and cirrhosis.
Etiology:
1- Conditioning for bone marrow transplantation with the use of cyclophosphamide, alkalating agents with or without total body irradiation. This is the major cause today for VOD. The onset of the disorder appears 3-4 weeks after transplantation and is seen in up to 20% of cases. Mortality rate is 50%.
2-Irradiation. This is the second most frequent cause. The lesion is dose relate and can occur with 10 Gy of irradiation with chemotherapy as in the case of bone marrow transplantation and with 30Gy without chemotherapy.
3-Antineoplastic drugs such as: azathioprine, 6-mercaptopurine, 6-thioguanine, mitomycin C,
BCNU(carmustine), vincristine, adriamycin. Some drugs, as azathioprine may cause the lesion many months after continuous administration.
4-Pyrrolizidine alkaloids. These compounds are found in about 300 species of plants such Heliotropium , Crotolaria and Senecio found all over the world and used to make herbal teas and enemas. The injury is due to the toxic effect of pyrrolic molecules on DNA of liver cells. Indeed the initial injury is necrosis of perivenular sinusoid with sinusoidal progressive occlusion, which is followed by fibrous occlusion of the central vein. This is the least frequent cause of VOD.
5-Other causes. Alcoholic liver; congenital immunodeficiency; dimethylnitrosamine; aflatoxin.
Distribution.
Endemic in Jamaica. Present in Egypt, South Africa, South America, India, Canada and Middle East where it is endemic among children who may demonstrate VOD and thrombosis of the large hepatic arteries.
Diagnosis.
Depends on clinical signs and on non-invasive imaging techniques, angiography and liver biopsy.
Prognosis.
There is 50% mortality in cases due to chemotherapy and irradiation. The majority of cases due to other natural causes recover. More than 50% of cirrhoses observed in Jamaica are due to VOD.
Treatment.
There is no specific treatment, only supportive measures.