These issues are best brought out by the following case studies:
A 19 year old woman with history of cocaine abuse brings her 12 month old child to your office for routine care. The child was born at 35 weeks and was partially worked up for failure to thrive early in his life. The workups were not completed due to many missed appointments and poor compliance. Today in your office, the child is very attached to his mother and cries when separated from her. He also seems withdrawn and not inquisitive of his surroundings.
On physical exam, you notice what appear to be bruises on his buttocks and back. When asked about them, the mother says that kids are just clumsy and he is always falling and getting hurt. When you probe more carefully into the bruises the mother becomes angry and defensive, telling you to just finish your job so that she can get home. You continue your physical exam with palpation and notice that the baby seems to have tenderness over his right back mid-thoracic ribs.
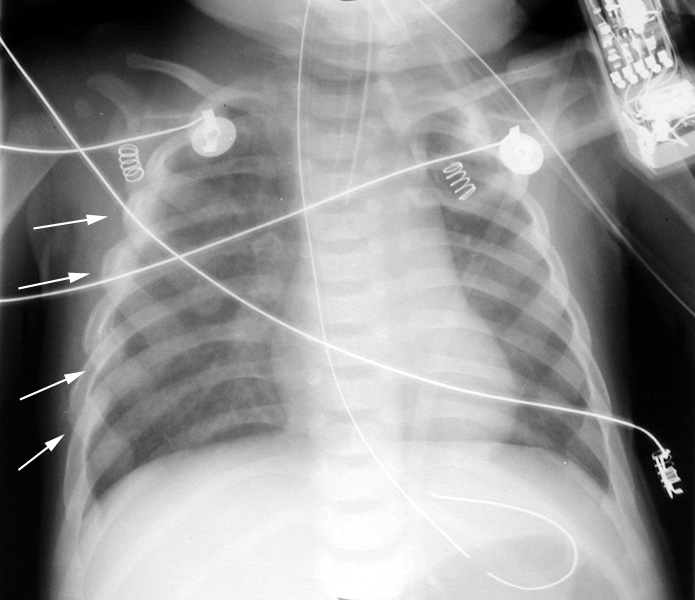
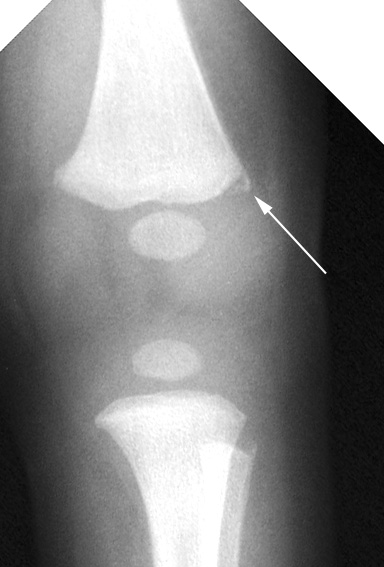
Suspecting abuse, you order an x-ray bone survey with multiple views of the skull, ribs, spine and extremities. On x-ray, the child has multiple rib fractures in different stages of healing, along with a left scapular fracture and a right thumb fracture. Finally, there is also a spiral fracture of the right femoral shaft.
 |
Rib films: multiple posterior rib fractures with callus |
 |
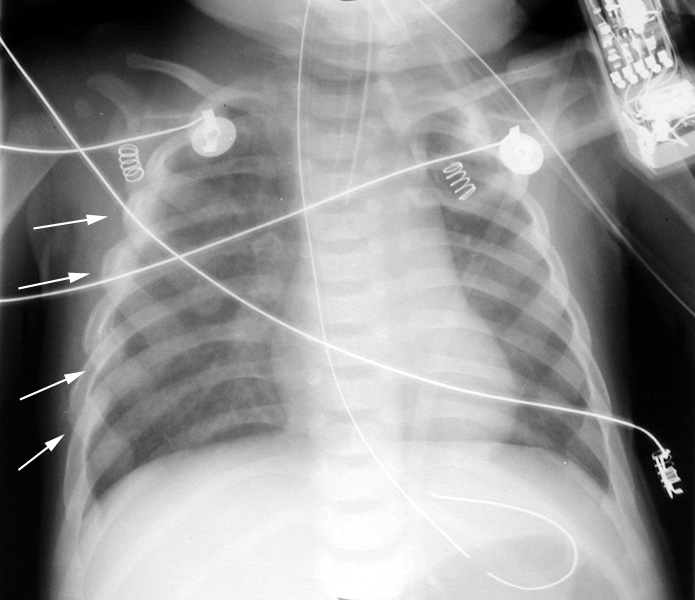
Tibia and fibula: arrowheads point to fracture that runs across metaphyseal width - bucket handle appearance. Arrow points to corner fracture of distal femur. |
|
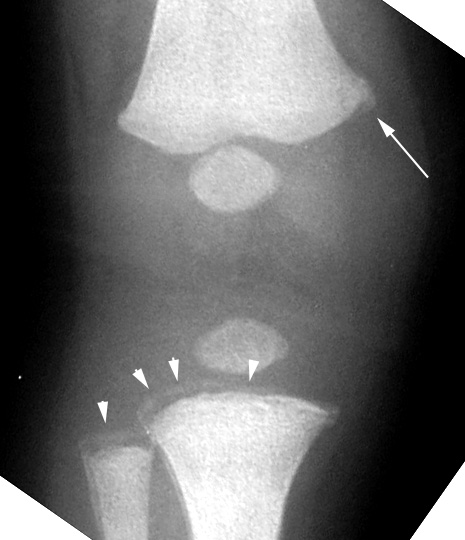
Femur: metaphyseal lipping of distal femur - corner fracture |
The x-ray findings are highly suspicious for abuse. Whenever a child has multiple fractures in different stages of healing, abuse should be suspected. Furthermore, the location of the fractures is very specific for abuse, especially the rib, scapular and finger fractures. Spiral fracture of the femur in a pre ambulating child is also very suspicious.
Child protective services must be contacted. A child in whom abuse is so probable should not be allowed to return to the unsupervised home before a complete workup is done. If no other safe situation is readily available, the child should be admitted for further work up.
Your next patient is a two-and-a-half year old child that you have been seeing since birth. She has model parents who seem very concerned about her. She presents today with both her parents who are concerned because she has been holding her left arm guardedly since this morning. They are afraid that she has broken her arm and are upset because she has broken her clavicle and her tibia since she started walking. She doesn't seem to be particularly clumsy and the parents deny any trauma.
On physical exam, you notice what appear to be bruises of various ages on her shins and forearms. She is guarding her left forearm and complains of tenderness to palpation over the distal radius. You also notice that her sclerae appear slightly blue. Upon further questioning of the parents, they say the bruises are from her exploring around the house and bumping into things. However, they are very concerned about her arm tenderness. When attempting to question the child, she does not have any particular recollection of hurting herself. She seems to be a happy, outgoing and entirely normal two year old.
While this case is not as suspicious as the first, it still warrants some work up. However, do you think a bone survey is necessary? Since the child is verbal and seems to answer all questions appropriately, a bone survey may not be completely necessary. However, this is a gray area. Being a very careful clinician, you do order a whole body bone survey, which shows a new left distal radius fracture along with healing fractures of the right tibia, right clavicle and possibly of the left tibia.
While this patient does have multiple fractures in various stages of healing, they are in locations that a child would normally fracture through routine trauma. Furthermore, none of the fractures involve the metaphysis. This does not paint a picture for abuse, but it is still suspicious. You question the parents more and they say that children in their extended families seem to fracture bones more often than most kids, but that they usually grow out of it by adolescence. You decide to do skin punch biopsy which helps you diagnose osteogenesis imperfecta type I.
A seven-month-old boy is brought to the emergency department by EMS. The boy is unresponsive and accompanied by his frantic parents. They say they do not know what happened. He has been otherwise healthy but they say that he had been playing in the family room when they found him in that condition. They say he may have fallen from the couch.
On physical exam he is afebrile and unresponsive - even to painful stimuli. On direct ophthalmoscopy you notice what appear to be retinal hemorrhages.
The boy is sent for a CT scan of the head. He is found to have a subdural hematoma. Neurosurgical consult is obtained and the boy is sent to the operating room for evacuation of the hematoma. While he is in surgery, you ask the parents more questions. They appear very nervous and become defensive on questioning. They maintain that the boy must have fallen from the couch.
A study has shown that a fall from three feet can rarely result in a simple fracture of the skull. From six feet, the child may have a concussion or, rarely, a small subdural hematoma. There have been no reported witnessed severe brain injuries from falls less than 10 feet. You suspect abuse, particularly traumatic shaking, and report the case to child protective services.
A six year old boy is brought to the emergency department with complaint of vomiting for one day. He denies any other symptoms and says nothing unusual has happened. He has not been able to hold down any food since yesterday. On physical exam his abdomen is distended and diffusely tender. You send routine laboratory studies which uncover elevated liver enzymes as well as a moderate amount of blood in the urine. Nasogastric tube decompression is done with some relief.
CT scan of the abdomen is obtained and shows dilated loops of small bowel with swelling at the proximal jejunum. The findings are consistent with blunt abdominal trauma and bowel wall hematoma causing obstruction.
After trying to establish a good rapport with the patient, you carefully try to comfort him and question him more carefully. When you tell him that his findings appear due to abdominal trauma, he tells you that he ran into the edge of a table the previous day. When you press him for details and question him more, he admits that he was hit in the abdomen by his father as a punishment for misbehaving.
Multiple bilateral fractures at different stages of healing: