|
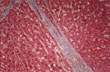
Fig.77 - MICRONDULAR CIRRHOSIS: Small rather uniform 2m nodules seperated by thin fibroussepta usually due to a chemicalagent as alcohol which diffuseuniformly throught the liver.
 |
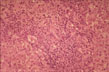
Fig.78 - MACRONODULAR CIRRHOSIS: Larger nodules separated by wider scars and irregularly distributed throughout the liver usually due to an infectious agent such as viral hepatitis which does not diffuse uniformly throughout the liver.
MICROSCOPIC CHANGES.
Presence of nodules and fibrous septa with effacement of the lobular architecture. The nodules are of two types: Dissection type and Hyperplastic Regenerative type.
 |
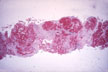
Fig.79 - DISSECTION NODULES:
- contain remnants of portal tracts an central veins.
- are separated by wide scars but contain thin fibrous septa.
- contain dilated sinusoids especially at their periphery looking like multiple central veins obviously produced by the inflow of arterial blood coming from the surrounding wide scars.
- the portal tracts within large nodules may be hypoplastic containing portal venule and arteriole but no bile ducts giving the impression of a disappearing bile duct disorder.
- within wide scars regenerative nodules may develop.
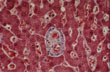 |
Fig.79a - HYPOPLASTIC PORTAL FIELD: In a dissecting nodule. Notice presence of portal vein, portal artery but no bile duct.This case was interpreted as "vanishing duct syndrome".
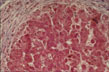 |
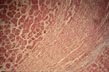
Fig.80 - REGENERATIVE NODULES:
- these occur in micro and macro nodular cirrhosis.
- they arise in the midst of scars favored by the rich arterial blood of scar tissue.
- they are round nodules with a fibrous pseudo capsule with bile ductules due to obstruction of bile flow.
- they have embryonal type of cell plates, two cells thick, "twinning of cell plates".
- nuclei are aligned at the sinusoidal pole of the plates.
- they often show focal cholestasis.
- they may undergo dysplastic and malignant changes.
- they compress the vessels of the capsule contributing to the perpetuation of the cirrhosis.