|
Aortic Dissection |
What is the classic clinical presentation of a dissecting aorta?
- Symptoms and clinical findings often depend on the extent and involvement of dissection.
- Abrupt and severe retrosternal or inter scapular chest pain is sometimes felt as a tear, with subsequent migration down the back occurs in 90% of patients.
- Classically, the pain is of maximal intensity at onset, unlike the pain of myocardial ischemia, which tends to crescendo and reach maximal intensity later.
- Complications of the dissection can produce additional signs and symptoms such as acute aortic insufficiency and pericardial effusion.
- Dissection can compress or occlude a branch of the aorta and produce acute ischemia.
- Ischemia occurs in the arms or legs in 20%, in the kidney in 15%, myocardium in 10%, brain in 5%, and mesentery or spinal cord in 3%.
- The patient will sometimes complain of exacerbation of the pain with each heartbeat.
- If the aortic arch is involved, patients may also feel pain in the jaw, neck, or teeth.
- In rare cases, patients may also be asymptomatic.
|
What is the common physical evidence for dissection?
- The loss of any pulse can occur with compromise to any major artery arising from the aorta.
- Aortic regurgitation can occur with disruption of the supporting structures of the aortic valve.
- Neurologic symptoms can occur with compromise of the head and neck vessels.
- In addition other physical findings may include: Horner's syndrome with compression of the superior cervical ganglion, vocal cord paralysis and hoarseness with pressure against the recurrent laryngeal nerve, superior vena cava syndrome, dyspnea secondary to tracheal or bronchial compression, hemorrhagic pleural effusion, and myocardial infarction as the hematoma dissects retrograde across the coronary ostium.
|
What are the predisposing factors?
Predisposing factors include those that increase stress on the arterial wall and those that reduce resistance on the arterial wall. These factors lead to acceleration of degenerative changes of the aortic media and increase the likelihood of a tear. Demographically, men are affected more often than women, and the peak incidence is at approximately 60 years of age.
The most common factors increasing stress on the arterial wall are:
- Hypertension
- Bicuspid aortic valve
- Aortic coarctation
- Iatrogenic (cardiac surgery and percutaneous catheters)
- Invading atherosclerotic plaque
The most common factors reducing resistance of the arterial wall are:
- Aging
- Connective tissue disorder's (Marfan's syndrome, Ehlers-Danlos syndrome)
- Aortitis (Syphilis, Giant Cell, SLE)
- Pregnancy
|
What is the classification of dissection of aorta?
DeBakey's Classification:
- Type I and type II dissections both originate in the ascending aorta.
- In type I, the dissection extends distally to the aortic arch.
- In type II, it is confined to the ascending aorta.
- Type III dissections originate in the descending aorta.
Stanford Classification:
- Type A includes all dissections involving the ascending aorta regardless of the entry site location.
- Type B dissections include all those distal to the left subclavian artery sparing the ascending aorta.
In addition, aortic dissection can be characterized as acute, lasting less than two weeks, or chronic, present for more than two weeks.
|
Diagnosis:
Aortic dissection is usually suspected from the history and physical exam. In a recent study, 96% of acute aortic dissections were identified based on a combination of the following three clinical features:
1) Immediate onset of aortic pain with a tearing and/or ripping character
2) Mediastinal and/or aortic widening on chest radiograph.
3) Variation in pulse and/or blood pressure between the right and left arm.
The incidence of dissection was:
- 7% when all three variables were absent.
- 31% and 39%, respectively, when either aortic chest pain or chest radiograph findings were present.
- >83% when a pulse or blood pressure differential or any two variables occurred.
- 100% when all three variables were present.
The optimal care of patients with aortic dissection requires that the diagnosis be made promptly, and the type of dissection be identified quickly. Most patients with type A dissections require surgery, while those with type B dissections can be successfully treated with medical management alone.
|
What are the imaging procedures available for evaluation of patients suspected to have dissection of aorta?
- For many years, the gold standard in diagnostic studies has been aortography, but recent literature has shown that other modalities may be more sensitive, specific, and practical.
- Current techniques available for evaluation include:
- CT angiogram
- Transthoracic echocardiography (TTE)
- Transeopsophageal echocardiography (TEE)
- MRI
- Aortography
|
How do you select the imaging procedure?
In deciding which study to select, one must consider what information is important to obtain. This may include the presence of:
- aortic dissection
- involvement of the ascending aorta
- extent of the dissection
- sites of entry and re-entry
- formation of thrombus in the false lumen
- any branch-vessel involvement or aortic insufficiency
- presence of pericardial effusion
- any coronary involvement.
Other important factors to consider include the accuracy of the diagnostic information, the availability of a test, the length of time involved, the safety, and cost.
|
Procedure Sequence/Diagnostic Algorithm
- There has been a shift from invasive (aortography) to noninvasive imaging studies to diagnose an aortic dissection.
- CT, MRI, and TEE are all effective imaging techniques for aortic dissection.
- Most patients end up having multiple imaging studies.
- The initial imaging study was
- CT - 61%,
- TEE - 33%
- aortography - 4%.
|
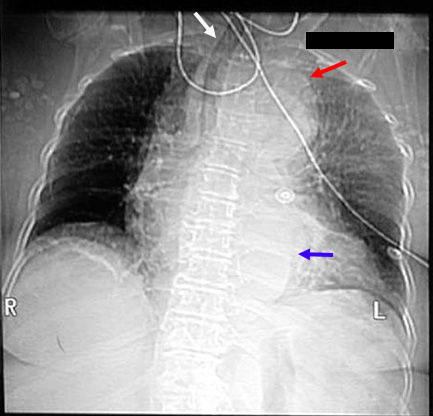
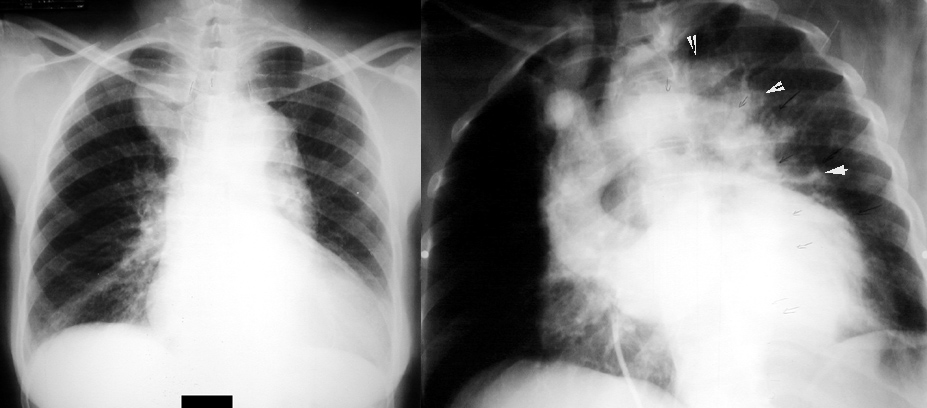
Radiologic Criteria for dissection in plain chest radiograph:
- Demonstrates mediastinal widening in around 63% of patients with an aortic dissection, however this finding is nonspecific and is seen in many normal age-matched controls.
- Internal displacement of aortic calcifications by 1 cm or more and disparity in size between the ascending and descending aorta are more specific for aortic dissection, especially when they represent a new finding compared to old films.
- Inlet to outlet shadow with wavy margins
- Frequently a left pleural effusion is seen.
- Localizes bulging of the aortic contour indicating the likely site of origin of a dissection.
|
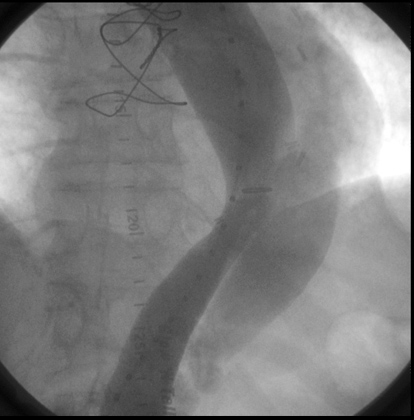
Radiologic Criteria for Dissection in Aortography:
- Aortography has long been considered the study of choice for evaluating suspected aortic dissection.
- It is performed by injecting the contrast agent retrograde through the femoral artery.
- The diagnosis of aortic dissection can be made on the basis of direct or indirect angiographic signs.
- The direct signs (which are diagnostic) include visualization of a double lumen or an intimal flap.
- The indirect signs (which are suggestive), include compression of the true aortic lumen by the false lumen, thickening of the aortic wall, or aortic insufficiency.
- Aortography is advantageous in that it can detect several complications including aortic insufficiency, involvement of the branch vessels, thrombus in the false lumen, and in some cases, involvement of the proximal coronary arteries.
- Aortography has a reported sensitivity of 88% and a specificity of 94%.
- In addition to its limited sensitivity, there are other disadvantages to aortography such as the risks involved with any invasive procedure requiring contrast.
- There is a high cost associated with aortography.
|
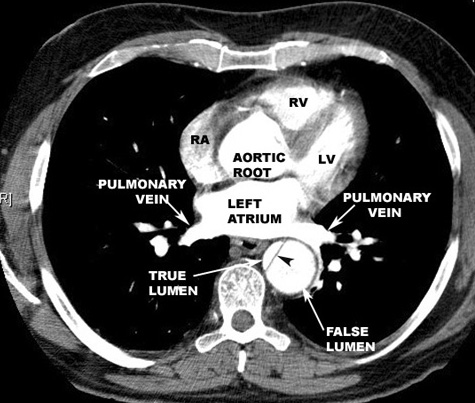
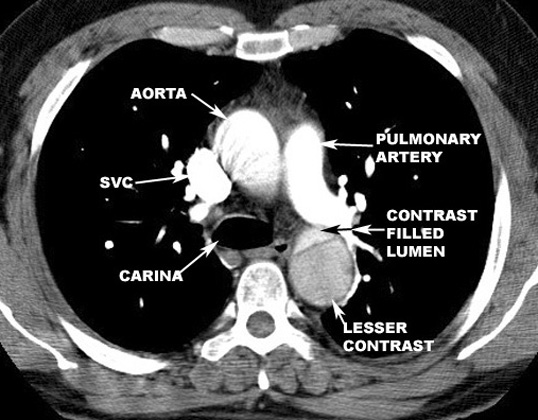
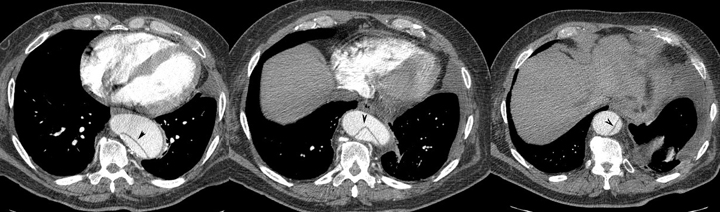
Radiologic Criteria for Dissection in CT scanning:
- The diagnosis of aortic dissection by CT requires the identification of two distinct lumens with a visible intimal flap:
- False lumen
- Flap
- True lumen
- Indirect signs include compression of the true lumen by the false lumen, spiraling of a thrombosed false lumen, displaced intimal calcification, widening of the aortic lumen, and ulcer-like projections of contrast material.
- The advantages of CT include ready availability and the fact that it is a noninvasive procedure.
- It is also helpful in identifying causes of aortic widening other than dissection (such as tumors or periaortic hematomas), and can identify the presence of a pericardial effusion.
- It is disadvantageous in that it cannot identify the presence of aortic insufficiency or delineate coronary arteries.
- Contrast-enhancing CT scanning has a reported sensitivity of 94%, but a specificity of only 87%.
- Current CT scanning techniques improve the accuracy of CT scanning in diagnosing aortic dissection.
- 3D reconstructed images provide remarkable details.
|
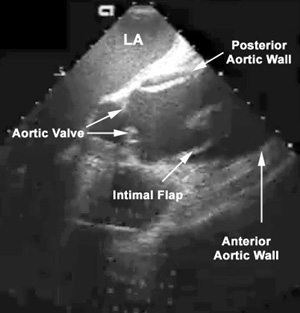
Radiologic Criteria for Dissection in Transthoracic and Transesophageal Echocardiography:
- The most definitive finding in diagnosing an aortic dissection by echocardiography involves visualization of an undulating intimal flap in the aorta.
- This intimal flap should be seen in more than one view, and should have a defined motion that is not parallel to the motion of any other cardiac or aortic root structure.
- The advantages of using echocardiography include easy availability and the fact that it is a quick, noninvasive procedure that can be done at the bedside.
- TEE may be capable of showing the ostia and proximal coronary arteries, and can be useful in detecting other cardiac problems if aortic dissection is excluded (ie: MI, ischemia, valvular vegetations, aortic stenosis, or pericardial tamponade).
- Echocardiography is disadvantageous in that TEE has difficulty visualizing the aortic arch, and cannot visualize the descending aorta very well.
- Also, the image quality of the TTE is adversely affected by obesity, emphysema, mechanical ventilation, chest wall deformities, or small inter costal space.
- In addition, the TEE is contraindicated in patients with known esophageal disease such as strictures or varices.
- Complications of TEE include bradycardia, AV block, hypertension, esophageal perforation, and bronchospasm.
- Due to visualization difficulties stated above, the specificity of TEE to be 77% (although sensitivity was 98%), and the specificity of TTE was only 68%.
- False positive tests were usually the result of reverberations from atherosclerotic vessels, a sclerotic aortic root, or calcified aortic disease producing echo images that resemble an intimal flap.
- The biplanar and multiplanar TEE may be of greater usefulness in increasing the specificity by providing additional views of cardiovascular structures in oblique planes.
|
Radiologic Criteria for Dissection in MRI:
- The criterion used to diagnose an aortic root dissection by MRI is also like those seen on CT.
- MRI is advantageous because it is noninvasive and requires no IV contrast.
- In addition, MRI can produce images in the transverse, coronal, sagital, and oblique planes of the aorta, which obviously facilitates the diagnosis of aortic dissection and provides a better definition of its location and extent.
- The disadvantage of MRI includes the fact that it cannot safely be performed in patients with pacemakers, certain types of aneurysm clips, metallic ocular implants, and certain types of metallic heart valve prostheses.
- MRI does not provide information about the imaging of the coronary vessels and the imaging of the arch vessels is poorer in quality than that obtained with aortography.
- Perhaps the most important limitation lies in that many patients with aortic dissections are hemodynamically unstable, and may not be able to tolerate being in an MRI machine for 15-65 minutes.
- MRI has a sensitivity and specificity of 98%. Thus although an MRI may be impractical for an unstable patient, the sensitivity and specificity make it the most useful test for diagnosing aortic dissection.
|
Pathophysiology
- Widening of aorta.
- Mass like density.
- Double lumen. True and false lumen.
- Displacement of Calcification of wall of aorta.
- Occlusion of branches arising from aorta.
- Rupture of aortic wall and escape of blood.
|