Ectopic Pregnancy
by
Molly Jonna, MS4 and Jennifer Lim-Dunham, M.D.
What are the imaging findings of ectopic pregnancy?
- An empty uterus with no gestational sac and a b-HCG level above a discriminatory level of 2000 mIU/ml is suspicious for an ectopic pregnancy.
- Sonographic adnexal findings that can be seen in a tubal ectopic pregnancy:
- Visualization of an adnexal mass separate from the ovary.
- The mass may be complex or contain a fluid filled gestational sac.
- A fetal pole may be present or absent.
- The embryo may or may not have cardiac activity, depending upon its gestational age and viability. If there is a detectable heartbeat the diagnosis is confirmed.
- The fallopian tube is the site of 98 percent of all ectopic gestations; 75 to 80 percent of implantations occur in the ampullary tubal segment, and therefore, imaging will visualize most ectopic pregnancies between the uterus and ovary.
- In addition, one may see free fluid. Peritoneal free fluid that is echogenic or complex is never physiologic, and in this clinical scenario almost always represents hemopertioneum from a ruptured ectopic.
- Ectopic pregnancies can be missed by US, when a tubal mass is small or obscured by bowel. With regard to sonographic identification of an ectopic pregnancy the sensitivity is 96% and the specificity is 99% when free peritoneal fluid is identified. When there is a tubal mass, the sensitivity is 81% and the specificity is 99%.
What are the useful modalities in evaluating ectopic pregnancy? What is the utility of each procedure?
- Transvaginal Pelvic Sonography
- Transvaginal and transabdominal pelvic ultrasonography are the initial modalities for evaluating a suspected ectopic pregnancy. Transvaginal pelvic sonography is more reliable at detecting early gestations. The scan can be useful as soon as 1 week after a missed menses with a serum b-HCG greater than 1500 mIU/ml. If an empty uterus with no gestational sac is seen with a b-HCG above 2000 mIU/ml, this is presumptive diagnosis of ectopic pregnancy. Identification of fetal heart action outside the uterine cavity is firm evidence of an ectopic pregnancy.
- Transabdominal Pelvic Sonography
- A transabdominal pelvic ultrasound is performed in conjunction with transvaginal pelvic ultrasound because it gives a larger field of view of the pelvis. One may be able to identify free fluid or an extra-ovarian adnexal mass. However, identification of pregnancy products in the fallopian tube is more difficult compared to transvaginal pelvic ultrasound. In addition, a uterine pregnancy is usually not recognized until 5 to 6 menstrual weeks or 28 days after timed ovulation.
- Color Doppler Sonography
- Color Doppler is used when performing pelvic ultrasonography as it identifies sites of increased vascularity. If vascular color is seen in a “ring of fire” pattern around a gestational sac in an extra-uterine location this supports the diagnosis of ectopic pregnancy.
Appropriateness Criteria:
The American College of Radiology has developed Appropriateness Criteria which are evidence-based guidelines that assist physicians in making the most appropriate imaging decisions for a wide variety of clinical conditions.
According to the Appropriateness Criteria for acute pelvic pain in the reproductive age female with positive beta hCG, both transvaginal and transabdominal pelvic ultrasonography should be inItial studies with Doppler used as an adjunct. If ultrasound is inconclusive or non-diagnostic, an MRI of the abdomen and pelvis can be performed. CT is not recommended due to radiation risk.
Link to women’s imaging criteria: http://www.acr.org/Quality-Safety/Appropriateness-Criteria/Diagnostic/Womens-Imaging
Link to imaging criteria for acute pelvic pain in the reproductive age group: http://www.acr.org/~/media/ACR/Documents/AppCriteria/Diagnostic/AcutePelvicPainReproductiveAgeGroup.pdf
What are the risk factors for developing ectopic pregnancy?
Any woman who is capable of being pregnant can have an ectopic pregnancy, >50% of women with ectopic pregnancies will have no significant risk factors.
Risk Factors include:
- Infertility treatment
- Prior ectopic pregnancy
- Prior pelvic inflammatory disease
- IUD in place
- Tubal abnormality
- Previous abdominal or tubal surgery
Ectopic pregnancy occurs with a prevalence of 1.4% and accounts for one-fourth of maternal deaths.
What is the clinical setting when you will consider ectopic pregnancy?
- Symptoms:
- Vaginal bleeding, a palpable adnexal mass, and pelvic pain make up the classic clinical triad; however, only 45% of patients will present this way.
- Abdominal pain radiating to the shoulder (referred pain) may be associated with ectopic rupture irritating the diaphragm
- The urge to defecate may be due to fluid in the posterior cul de sac from ectopic rupture
- Physical findings:
- 75% abdominal tenderness, +/- rebound tenderness
- 66% cervical motion tenderness
- 50% palpable adnexal mass
- 20% hemodynamic compromise (orthostasis, hypotension, shock)
- Often unremarkable findings if the ectopic pregnancy is small and unruptured
Take Home Points:
- Consider ectopic pregnancy in any woman with vaginal bleeding, abdominal pain, and positive pregnancy test
- In ectopic pregnancy, the expected gestational sac in the endometrial cavity of the uterus is absent when the beta hCG is above the discriminatory level of 2000 mIU/ml, and there may be a gestational sac with possible fetal cardiac activity in the fallopian tube or ovary.
- Blood or fluid in the space between the vagina and rectum in this clinical scenario indicates ruptured ectopic pregnancy
Imaging
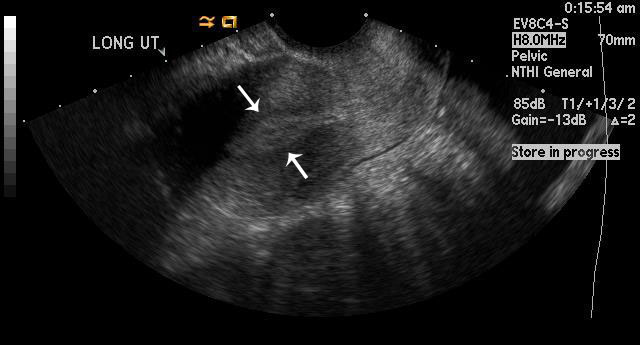 |
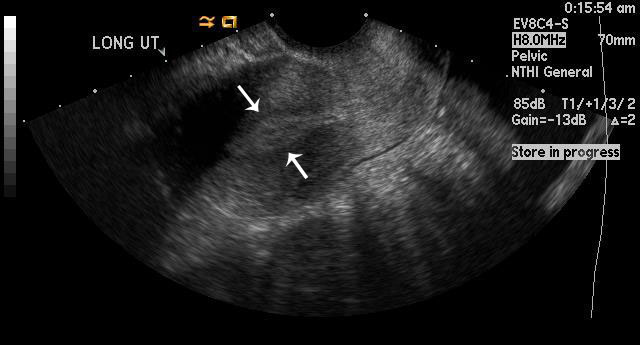
Figure 1
Uterus is empty with no gestational sac, which is concerning for ectopic pregnancy in this patient with a b-HCG level above 2000 mIU/ml. The arrows outline a central hyperechoic area that represents the normal endometrial stripe. |
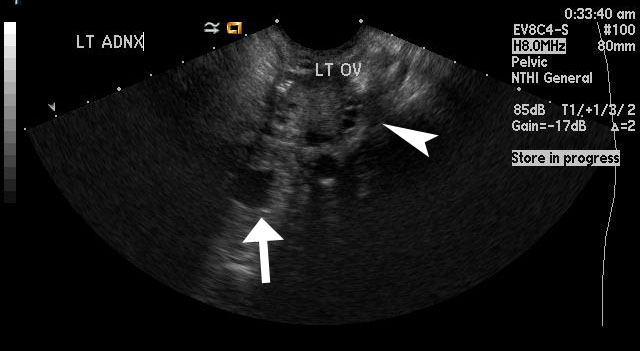 |
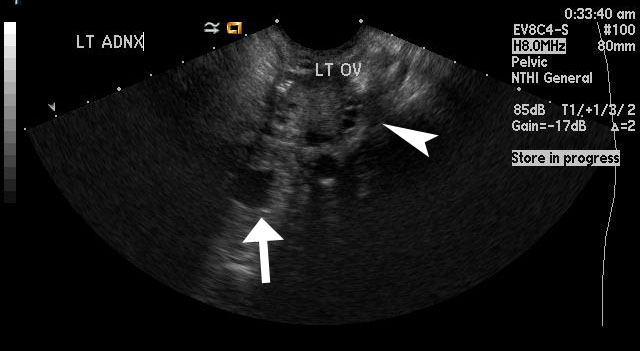
Figure 2
This image shows left adnexal ectopic pregnancy with the arrow pointing towards the anechoic gestational sac, which is separate from the left ovary (arrowhead). |
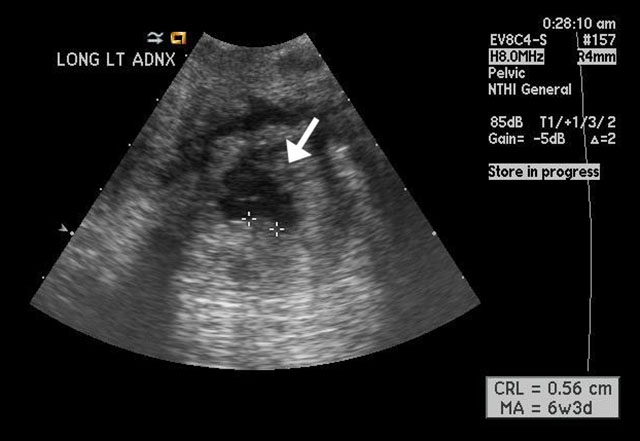 |
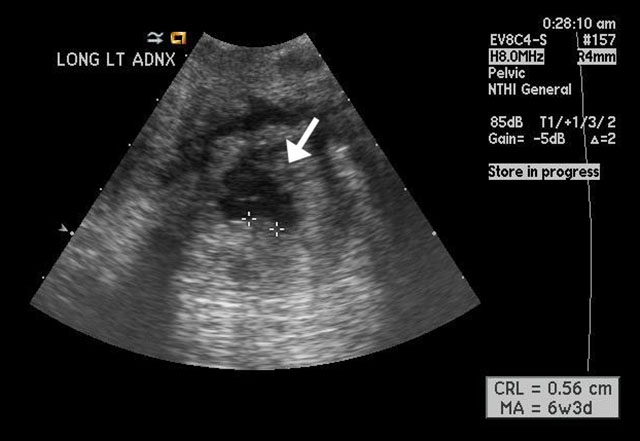
Figure 3
Magnified image shows the ectopic pregnancy in the left adnexa with the arrow pointing towards a fluid filled gestational sac that is anechoic. The calipers are measuring a hyperechoic area within the gestational sac, which most likely represents a fetal pole. |
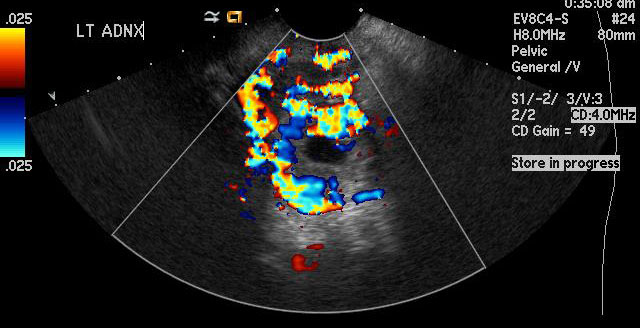 |
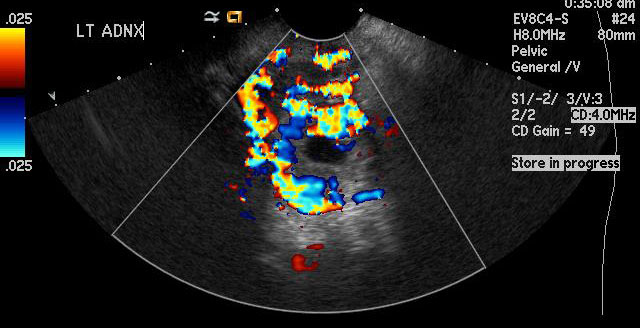
Figure 4
This image has color Doppler which shows increased vascularity in the left adnexa in a ring-like pattern concerning for an ectopic pregnancy |
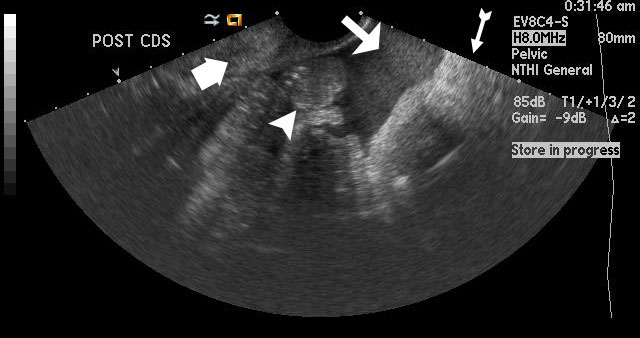 |
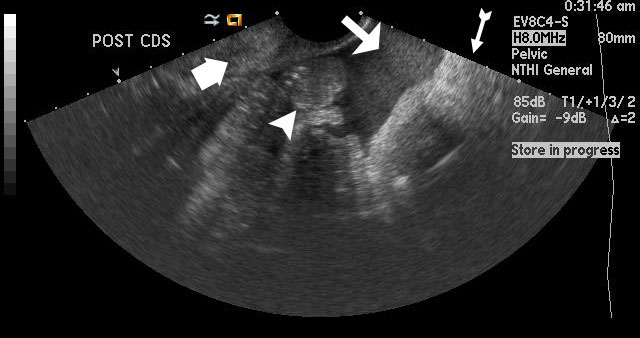
Figure 5
Medium-sized arrow shows echogenic free fluid representing hemorrhage in the posterior cul-de-sac in this patient with ectopic pregnancy. The thin arrow with a tail points toward a hyperechoic structure that is the rectum, and the thick arrow points towards the cervix. The arrowhead is pointing out hyperechoic structures, which are bowel loops. |
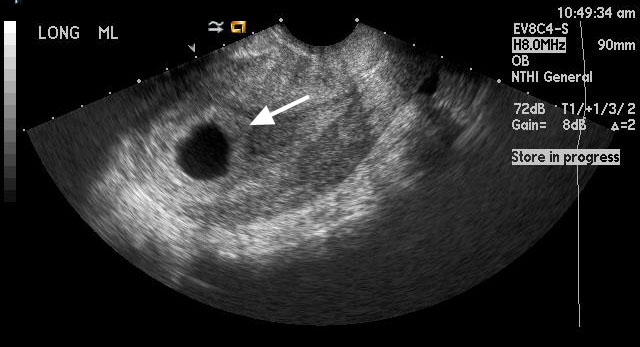 |
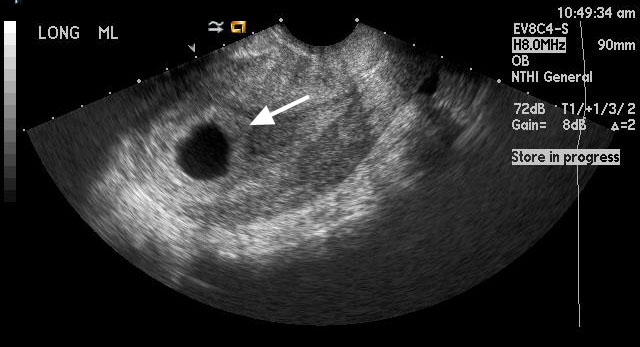
Figure 6
For comparison, this image shows a normal intrauterine pregnancy at 6 weeks gestation. The arrow points to an anechoic fluid filled gestational sac within the uterus. You can note the decidual reaction which is the hyperechoic area surrounding the gestational sac. |
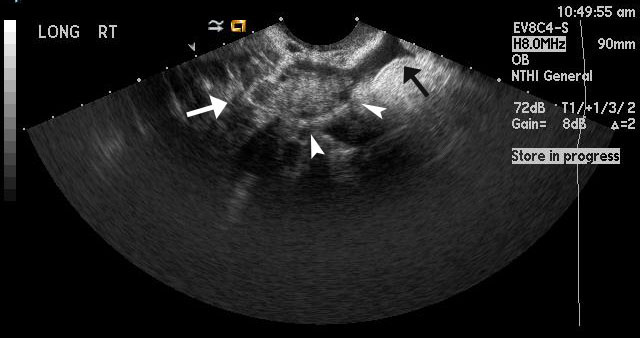 |
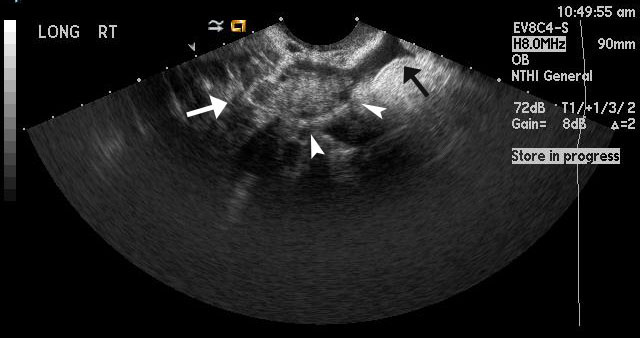
Figure 7
For comparison, this image shows a normal right ovary. The white arrow points towards the ovary. The arrowheads point towards hypoechoic round structures, which represent normal follicles. The black arrow indicates a small amount of physiologic, anechoic free fluid, (no echogenicity or complexity). |
Helpful Links with More Imaging:
- http://emedicine.medscape.com/article/403062-overview#a22
- http://www.med-ed.virginia.edu/courses/rad/edus/pelvic3.html
References:
- Levine, D. (2007). Review for residents: Ectopic pregnancy. Radiology, 245(2), 385-397. Retrieved from http://pubs.rsna.org/doi/full/10.1148/radiol.2452061031
- Tejas, M. S. (2013). Ultrasonography of pregnancy of unknown location. In S. Falk (Ed.), UpToDate. Retrieved from http://www.uptodate.com/contents/ultrasonography-of-pregnancy-of-unknown-location?source=see_link
- Williams, P. L., Laifer-Narin, S. L., & Ragavendra, N. (2003). US of abnormal uterine bleeding. RadioGraphics, 23, 703-718. Retrieved from http://pubs.rsna.org/doi/full/10.1148/rg.233025150
11/22/13