Pelvic Inflammatory Disease/Pyosalpinx
by
Molly Jonna, MS4 and Jennifer Lim-Dunham, M.D.
What is pelvic inflammatory disease?
- Pelvic inflammatory disease (PID) is an acute infection of the upper genital tract structures in women; it can involve the uterus, oviducts, ovaries and neighboring pelvic organs. This results in endometritis, salpingitis, oophoritis, peritonitis, perihepatitis and tubo-ovarian abscess, of which pyosalpinx can be a component. Pyosalpinx is inflammation of the fallopian tube that results in adhesions and obstruction of the fimbrial end. The fallopian tube is unable to drain and so it distends with pus.
- Chlamydia trachomatis and Neisseria Gonorrhae are most commonly responsible for the acute infection when sexual transmission has taken place. Staphylococci, streptococci or coliforms are the most likely organisms in cases not related to sexual transmission. However, regardless of the initiating event, the microbiology of PID, especially for clinical purposes, should be viewed and treated as a mixed (facultative and anaerobic) polymicrobial infection.
What are the useful imaging modalities in evaluating PID?
What is the utility of each procedure?
- Pelvic Ultrasound:
- Sonographic findings consistent with PID, especially thickened, fluid-filled oviducts, are useful to support a clinical diagnosis of PID. However, the absence of findings does not diminish the probability of PID and should not be used as a reason to delay treatment.
- An ultrasound is indicated, if an adnexal mass is suspected, the diagnosis is in question, or if the patient does not respond to initial therapy.
- Ultrasound is sensitive and specific for the presence of tuboovarian abscess.
- Transvaginal US allows for better definition of pelvic anatomy and should be performed in conjunction with transabdominal US
- CT:
- If the diagnosis is uncertain after pelvic US, CT can be useful, especially because it can demonstrate other pathology in the abdomen and pelvix.
- PID can often be confused with appendicitis, especially if cervical culture is negative.
Appropriateness Criteria
- The American College of Radiology has developed Appropriateness Criteria which are evidence-based guidelines that assist physicians in making the most appropriate imaging decisions for a wide variety of clinical conditions.
- According to the Appropriateness Criteria for acute pelvic pain in the reproductive age female both transvaginal and transabdominal pelvic ultrasonography should be initial studies with Doppler used as an adjunct. If ultrasound is inconclusive or non-diagnostic, an MRI of the abdomen and pelvis can be performed. CT is not recommended due to radiation risk.
- If the female is known to be non-pregnant, the recommendations for acute abdominal pain with fever or a suspected abdominal abscess is to use CT as the primary imaging modality as it is quick in an emergency setting and helpful in both ruling in and ruling out other disease processes.
Link to women’s imaging recommendations:
http://www.acr.org/Quality-Safety/Appropriateness-Criteria/Diagnostic/Womens-Imaging
Link to imaging criteria for acute pelvic pain in the reproductive age group:
http://www.acr.org/~/media/ACR/Documents/AppCriteria/Diagnostic/AcutePelvicPainReproductiveAgeGroup.pdf
Link to imaging recommendations for acute abdominal pain and fever or suspected abdominal abscess:
http://www.acr.org/~/media/ACR/Documents/AppCriteria/Diagnostic/ AcuteAbdominalPainFeverSuspectedAbdominalAbscess .pdf
What are the imaging findings of PID?
Ultrasound
- Pyosalpinx- fallopian tube can be seen as a dilated serpentine/tubular structure in the pelvis separate from the ovary that is filled with echogenic complex fluid, which represents pus. Low- level echoes represent the higher protein content of the debris within the tube and a fluid-debris level may be seen. Pelvic inflammation may be seen as an ill-defined uterus and increased echogenicity of pelvic fat.
- Tubo-ovarian abscess –If the infectious process progresses beyond the fallopian tube to involve the ovary, the two structures cannot be identified as discrete entities and together form a tubo-ovarian complex. The tubo-ovarian abscess appears as a solid and cystic adnexal mass containing debris and complex fluid.
- Small amounts of free pelvic fluid may be present due to PID adhesions
CT
- Pyosalpinx- tubular juxtauterine mass with complex internal fluid and thick enhancing walls
- Tubo-ovarian abscess- solid/cystic adnexal mass, with area of low attenuation and enhancement of the wall and septa
- Obscuration of normal pelvic floor fascial planes
- Thickening of uterosacral ligaments
- Accumulation simple fluid in endometrial canal/fallopian tubes/pelvis that may become complex fluid as the disease progresses
- Reactive inflammation of adjacent structures that manifests as pelvic fat stranding
What is the procedure of choice?
- PID is a clinical diagnosis, but the procedure of choice is transvaginal pelvic ultrasound.
- Diagnostic algorithm:
- If the patient has the clinical signs of PID give antibiotic treatment.
- If patient fails to respond to antibiotics, or there is a suspicion of pelvic abscess, then proceed with pelvic ultrasound.
- If the diagnosis is in question due to non-specific symptoms, and the patient is not pregnant, give antibiotics, and proceed with CT scan of the abdomen and pelvis.
What are the risk factors for acquiring PID?
The risk factors for acquiring PID are similar to those for acquiring an STD and include:
- Age less than 25 years
- Young age at first sex
- Nonbarrier contraception
- New, multiple, or symptomatic sexual partners
- Oral contraception
Factors that potentially facilitate PID include:
- Previous episode of PID
- Sex during menses
- Vaginal douching
- Bacterial vaginosis
- Intrauterine device
What is the clinical setting when you will consider PID?
Minimum criteria needed for clinical diagnosis:
- Lower abdominal tenderness- cardinal symptom
- Adnexal tenderness
- Cervical motion tenderness
Additional criteria, which increase the specificity of the diagnosis
- Oral temp >101
- Abnormal cervical or vaginal discharge
- Abnormal uterine bleeding
- Elevated ESR
- Dyspareunia
- Onset of pain shortly after menses
- Cervical infection with N. gonorrhea or C. trachomatis
Take Home Points:
- Pelvic inflammatory disease (PID) refers to acute infection of the upper female genital tract structures. It is considered a polymicrobial infection.
- Cervical motion tenderness or uterine or adnexal tenderness with lower abdominal or pelvic pain are the minimum diagnostic criteria.
- Diagnostic tests for PID include looking for signs of inflammation with ESR and white count, microscopic examination and cultures of cervical or vaginal secretions, and imaging studies.
- Laboratory testing for patients suspected of PID should include a pregnancy test to rule out ectopic pregnancy or complications of an intrauterine pregnancy.
- Pelvic US useful in acutely ill patients with PID when there is concern for a pelvic abscess.
- US findings can include tubo-ovarian abscess, pyosalpinx, and small amounts of fluid
- CT findings can include a fluid filled adnexal mass with reactive inflammation of adjacent structures.
Imaging
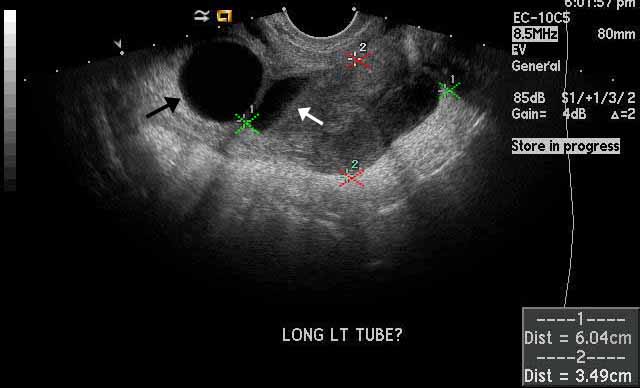 |
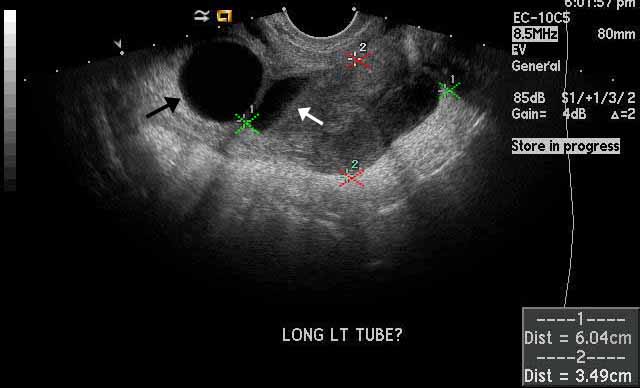
Image 1
Left pyosalpinx. The left fallopian tube, which is marked by the red and green calipers, is dilated and contains anechoic, simple fluid as well echogenic debris representing pus. The white arrow is pointing towards a fluid-fluid level. The black arrow is pointing to an anechoic cyst within the left ovary, which is adjacent to but separate from the dilated fallopian tube. |
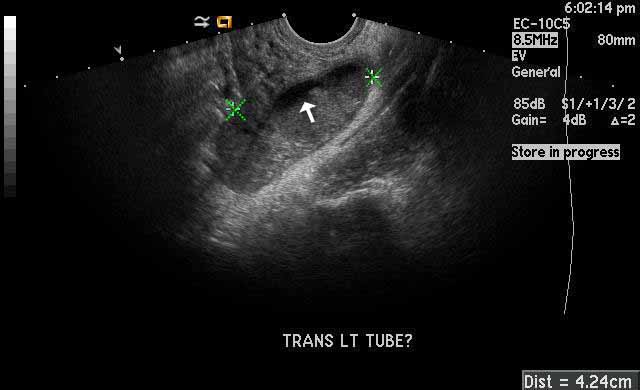 |
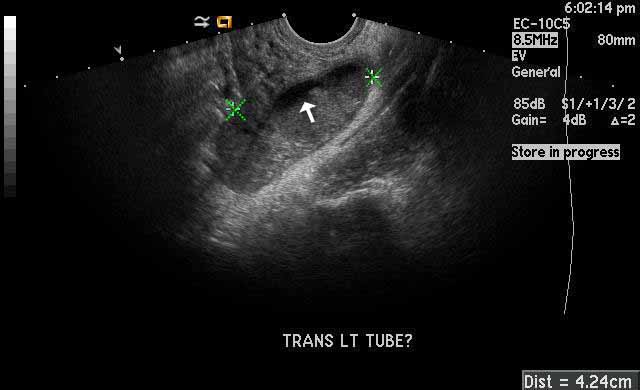
Image 2
Left pyosalpinx. The green calipers mark the dilated fallopian tube filled with anchoic fluid and echogenic pus. The white arrow is pointing towards a fluid-fluid level. |
|
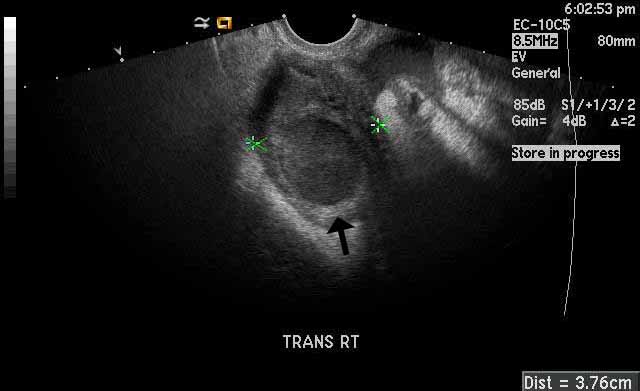
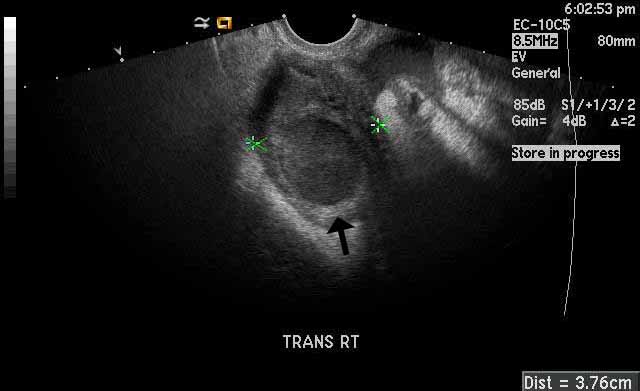
Image 3
Right tubo-ovarian abscess. The black arrow points towards a hypoechoic structure representing a combined complex collection encompassing both fallopian tube and ovary. Note that the abscess, marked by the green calipers, is characterized by a thick wall and central echogenic fluid representing pus. |
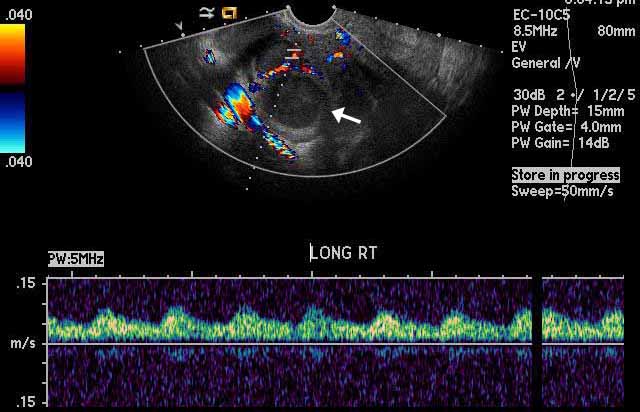 |
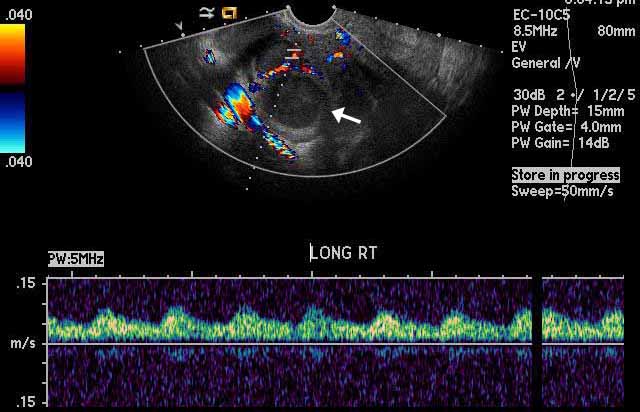
Image 4
Right tubo-ovarian abscess. Color Doppler shows that there is no flow within the hypoechoic right adnexal structure ( white arrow ) that represents the abscess. This indicates that the structure is a fluid filled mass as opposed to a solid mass. |
Helpful links with Additional Imaging:
- http://www.med-ed.virginia.edu/courses/rad/edus/pelvic2.html
- http://www.learningradiology.com/lectures/facultylectures/pidpptmh_files/v3_document.htm - a powerpoint of information and images that you can scroll through
- http://pubs.rsna.org/doi/pdf/10.1148/rg.312105090 - article with several images included, this is also linked in the references section
References
- Livengood, C. H., & Chacko, M. R. (2012). Clinical features and diagnosis of pelvic inflammatory disease. In N. Hynes & A. Bloom (Eds.), UpToDate. Retrieved from http://www.uptodate.com/contents/clinical-features-and-diagnosis-of-pelvic-inflammatory-disease?source=search_result&search=Pelvic+Inflammatory+disease&selectedTitle=2%7E150
- Rezvani, M., & Shaaban, A. M. (2011). Fallopian tube disease in the nonpregnant patient. RadioGraphics, 31, 527-548. Retrieved from http://pubs.rsna.org/doi/pdf/10.1148/rg.312105090
- Sam, J. W., Jacobs, J. E., & Birnbaum, B. A. (2002). Spectrum of ct findings in acute pyogenic pelvic inflammatory disease. RadioGraphics, 22, 1327-1334. Retrieved from http://pubs.rsna.org/doi/pdf/10.1148/rg.226025062
Case 1
A 26-year-old female presents to you in the STD clinic with a complaint of fever of three days duration, nausea, and lower abdominal pain. She denies a history of dysuria, hematuria, or genital ulcerations. She denies that she may be pregnant. She has an intrauterine device for 2 years. She takes no prescribed medications and she has no allergies. On examination, she has a temperature of 39 0 C, pulse rate of 110 per minute, respiration rate of 28 per minute, and B/P of 100/60. She is ill appearing and diaphoretic. There is no lymphadenapathy. She has right lower quadrant tenderness to deep palpation. Bowel sounds are present but hypoactive. Her pelvic examination reveals right adnexal tenderness and cervical motion tenderness. The uterus is tender and slightly enlarged. Thick yellow vaginal discharge is sent for microbiological studies. Pregnancy test is negative.
Question: Does she need imaging studies? Can she be treated empirically?
Answer: Yes.
Empiric treatment of PID should be instituted on the basis of the presence of all of the following three minimum clinical criteria for pelvic inflammation and in the absence of an established cause other than PID: 1) lower abdominal tenderness, 2) adnexal tenderness, and 3) cervical motion tenderness.
For women with fewer clinical signs, more elaborate diagnostic evaluation is warranted because incorrect diagnosis and management may cause unnecessary morbidity.
Case 2
19 year old sexually active girl presents with right lower quadrant pain and fever. Her LMP was one week back. She does not practice protective sex. She has right lower quadrant abdominal tenderness with rebound. On pelvic exam, there is some mucoid discharge from cervix. Uncertain about tenderness on cervical motion. Surgeon is debating between PID and appendicitis.
Question: Does she need any imaging procedure. If so which imaging procedure?
Answer: When you are uncertain of the diagnosis, imaging procedure should be utilized. CT would be the choice in this case as it will provide information about pelvis and abdomen. But pregnancy test must be done to rule out pregnancy before CT.
Case 3:
Patient is a 17-year-old sexually active G0P0 who comes to her primary care physician complaining of severe abdominal pain for 2 days. Her LMP was 2 weeks ago. She states that she uses condoms for contraception. Pt has a fever to 101. She has a tender lower abdomen, but no rebound or guarding. On pelvic exam, the patient has a purulent cervical discharge. Patient has a positive chandelier sign (cervical motion tenderness) as well as bilateral adnexal tenderness. B-HCG is negative.
This patient has Fitz-Hugh Curtis syndrome, which is perihepatits, a complication of untreated PID. One can see fluid around GB on ultrasound
12.17.13